In this section : Infectious Diseases
Treatment of Malaria
Gentamicin Prescribing (Paediatrics)
Influenza A
HIV Testing Guidelines
Clostridiodes difficile Infection
Blood Culture
OPAT SBAR (Complex Infections)
Staphylococcus aureus Bacteraemia (SAB)
Neutropenic Sepsis
Antibiotics and the Kidney
Acute Diarrhoea
Suspected Meningitis
Suspected Sepsis
Gentamicin Dosing
Urinary Tract Infection
Vancomycin Dosing
Cellulitis
Post Splenectomy Sepsis
Home | Articles | Infectious Diseases |
Treatment of Malaria
Last updated 10th May 2023
Malaria should be suspected in any patient with a fever/ history of fever who has returned from or previously visited a malaria endemic area even if they have taken malaria prophylaxis. It is essential to obtain information on the country and area of travel (including any stop-overs) and details of any malaria prophylaxis regimen (including drug choice, dose, adherence etc).
Patients with falciparum malaria generally present within a month of returning from the tropics but 10% of cases present up to 3 months after travel.
| Key Points 1. All patients with malaria/ suspected malaria should be referred to ID & micro consultant. There is no OOH ID service within NHS D&G. Suspected cases should be discussed with duty microbiologist if diagnosis of malaria is suspected. VHF risk assessment and appropriate IPC precautions should be considered. 2. Malaria is a medical emergency within the UK (i.e., immediate admission and malaria tests) 3. Non-immune individuals may clinically deteriorate rapidly (within hours) compared to those with partial immunity. 4. Patients with severe falciparum malaria can deteriorate rapidly so involve ICU early. Diagnosis/Testing: 1. Haematology BMS will require that a Viral Haemorrhagic Fever (VHF) risk assessment is performed before they can proceed with the malaria tests. This is because (if higher risk) the blood films may have to be prepared in the Cat 3 lab within microbiology and (out of hours) this will involve the duty micro BMS coming into hospital. 2. Rapid antigen diagnostic test (RDT) for malaria only takes about 20min to perform and can be performed by Haematology BMS 24/7/365. RDT is as sensitive/ specific as thick film for P. Falciparum, but less so far for other species. 3. Thick and thin blood films are the gold standard investigation for malaria, but it takes longer to prepare, stain and examine for speciation of malaria and parasite counts. Speciation may require delay until Consultant Haematologist review. 4. 3 negative diagnostic samples, with 12-24 hours between samples, are necessary to exclude malaria. 5. Bacterial co-infection is uncommon in adult travellers but should be considered when a malaria patient presents with shock or with focal signs such as pulmonary consolidation 6. Any uncertainty over infecting species should be treated as falciparum malaria. Treatment: 1. In severe/complicated falciparum malaria, IV artesunate is the drug of choice (if necessary, start IV quinine until IV artesunate is available) 2. Uncomplicated falciparum malaria and non-falciparum malaria should be treated with Riamet® |
Presentation
- Symptoms may include; fever/ sweats/ chills, lethargy, malaise, nausea, vomiting, abdominal pain, diarrhoea, myalgia, hepatomegaly and splenomegaly.
- Even patients with low parasitaemias can develop complications. Immunity wanes rapidly when patients move from endemic areas and we recommend that all patients presenting to UK hospitals are considered ‘non-immune’. Age is an independent predictor of poor outcome.
Indicators of Severe Malaria
- Cerebral involvement:
- May manifest as drowsiness, confusion, stupor, fits or coma – even mild drowsiness or confusion should be regarded as showing possible cerebral involvement
- Exclude hypoglycaemia
- Convulsions should be controlled with benzodiazepines
- Status epilepticus should be managed with anti-convulsants, but beware of potential interactions if
using quinine
- Anaemia
- Severe anaemia is uncommon in travellers but common in African children
- It is primarily due to haemolysis
- Correct Hb ≤80g/L with packed cells and monitor fluid balance, taking care not to overload
- Metabolic and lactic acidosis (pH <7.3)
- Acidosis is common and predictive of a poor prognosis
- Renal Failure
- Defined as an urine output 265 micromol/L
- Hyponatraemia is common in malaria and does not usually require correction
- Consider early haemofiltration or dialysis
- Pulmonary Oedema
- Correction of hypovolaemia should be carried out with caution
- Hypoglycaemia (<2.2mmol/L)
- In adults, particularly in pregnancy, this is due to quinine stimulating insulin release
- Hypovolaemia/ Shock
- Dehydration requires careful clinical assessment
- Secondary bacterial infection is possible
- Bleeding/ DIC
- Thrombocytopenia is almost invariable and is not necessarily an indication of severity although very
- low platelet counts (<50x 109/L) tend to predict severe disease
- Platelet transfusions are only indicated if there is evidence of bleeding and a very low count
- Beware early DIC and check clotting, fibrinogen and D-Dimer in severe malaria
- Jaundice
- Jaundice alone is not an indication for parenteral treatment
Investigations
- RDT antigen test/ Malaria blood test (thick and thin blood smears by microscopy) and Malaria parasites/ **antigen test
- RDT antigen tests are simple but have three main problems:
- they are less sensitive than microscopy
- they rely on detecting parasite antigen rather than live parasite and may therefore be positive in patients who have been recently treated (up to 2 weeks) or come from a malaria endemic area and have a low level of asymptomatic parasitaemia
- it is not possible to determine the parasitaemia or stage of parasite
- If there is high clinical suspicion of malaria but initial blood films are negative, repeat the malaria blood test after 12 – 24 hours and again at 48 hours
- Urea and Electrolytes, Full Blood Count, Blood Glucose, Liver Function Tests and Blood culture(s) for typhoid and/ other bacteraemia should be considered
- Urine dipstick (for haemoglobinuria) and culture. If the patient has diarrhoea, send faeces for microscopy and culture
- Chest radiograph especially in breathless patients & to exclude community acquired pneumonia
Classification of Severity
UNCOMPLICATED
- Parasitaemia ≤2% & no schizonts (on blood film) and no clinical Complications
SEVERE
- Parasitaemia >2%
- or Parasitaemia ≤2% with schizonts reported on blood film
- or Parasitaemia ≤2% with complications (see ‘Indicators of severe malaria’)
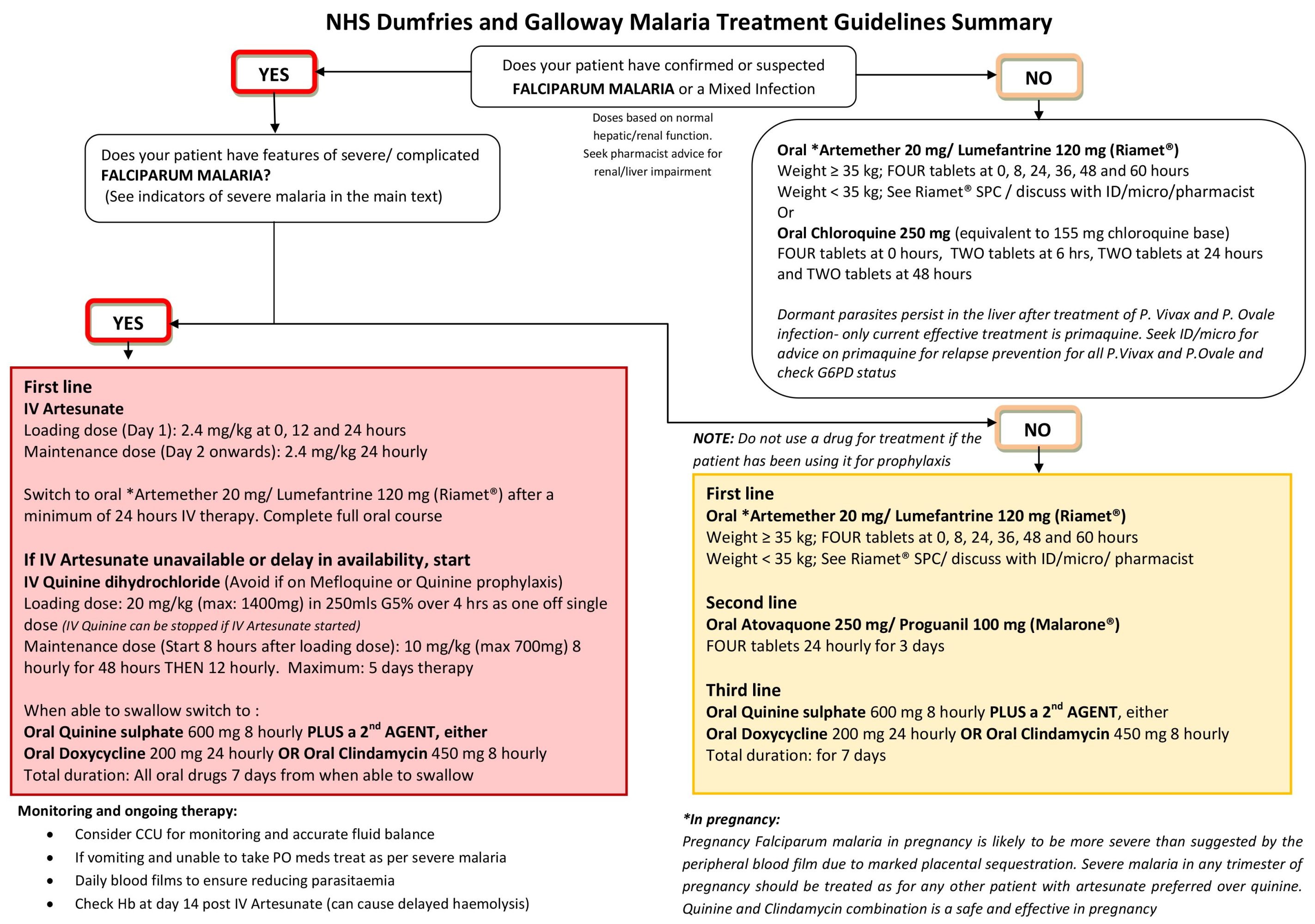
Treatment (refer to algorithm below)
Additional prescribing points (these are not exhaustive; See BNF, Summary of Product Characteristics (SPC), contact pharmacist.
| IV Artesunate and IV Quinine dihydrochloride | Artesunate has few side effects and there is no need to adjust for renal impairment or to monitor for cardiac toxicity. It does not promote hypoglycaemia. Has Rapid parasite clearance. Normally well tolerated, although post treatment haemolysis is recognised. IV Quinine can cause cinchonism (vertigo, tinnitus, visual blurring and nausea), may also prolong QT and cause hypoglycaemia- monitor |
| Riamet® | Riamet® may prolong the QTc interval. Avoid in patient with other risk factors for QTc prolongation Take Riamet® with food or drinks rick in fat such as full fat milk to maximise absorption Avoid Riamet® in the first the first trimester Occasionally, and particularly in patients with reduced ability to clear parasites (e.g. hyposplenism), a longer course may be required |
| Chloroquine | Chloroquine may prolong the QTc interval. Use with caution in patients with other risk factors for QTc prolongation. Patients with epilepsy should not be prescribed chloroquine. |
| Doxycyline | Avoid in all trimesters of pregnancy |
| Primaquine | G6PD status must be determined before prescribing Primaquine. Avoid in all trimesters of pregnancy. |
Content by Evelyn Yoong