In this section : Cardiac
: Palliative Care
Deactivation of Implantable Cardioverter Defibrillator
Palliative Care – How to Refer
Conversion Charts
Anticipatory ‘As Required’ Medications
Syringe Driver Chart
Scottish Palliative Care Guidelines
Breaking Bad News by Telephone
End of Life Diabetes Care
Fentanyl Patches in the Last Days of Life
Care in the Last Days of Life
Symptom Control
Deactivation of Implantable Cardioverter Defibrillator
Last updated 2nd February 2024
Background
- Defibrillators are implanted to provide treatment for life threatening rhythm disturbances such as ventricular tachycardia (VT) or ventricular fibrillation (VF). Treatment can consist of anti-tachycardia pacing (ATP) or cardioversion/defibrillation (shocks).
- There are two types of implantable defibrillator; ICD (implantable cardioverter defibrillator) and CRT-D (cardiac resynchronisation therapy – defibrillator). ICDs are generally implanted in patients in whom our primary concern is rhythm management. CRT-Ds are generally implanted in patients in whom there is significant impairment of left ventricular (LV) systolic function as well as a potential or actual rhythm problem. Both devices can also provide treatment to prevent bradycardia. (A CRT device may be implanted for LV systolic impairment with pacemaker function but without defibrillator capacity in which case this is called CRT-P). Please see appendix one for more information on ICD and CRT-D.
- Although deemed to be beneficial at the time of implant, the burdens of the aging process and or development of end stage cardiac disease or another life limiting condition may bring in to the question the continuing benefit of the full range of therapy which can be delivered by an ICD/CRT-D. With the exception of patients with ongoing myocardial ischaemia, the emergence of ventricular tachycardia (VT) or fibrillation (VF) as the mode of death in end stage cardiac disease/other life limiting condition is unlikely. Therefore it is possible for ICD/CRT-D to remain active until death. In a palliative care or end of life setting it becomes increasingly important for patients and families to have the opportunity to discuss the appropriateness of defibrillator therapies. For some patients deactivation should be considered as therapies may be associated with physical and emotional discomfort to the patient and distress to families and may no longer be successful.
In Which Situations Should Deactivation be Considered?
- ICD/CRT-D deactivation should be considered in all patients deemed to be in the last year of life. This will include patients whose death is imminent (expected in hours to days) and also those with: –
- Advanced, progressive, incurable conditions
- General frailty and co-existing conditions that mean they are expected to die within 12 months
- Existing conditions if they are at risk of dying from a sudden acute crisis in their condition
- Life-threatening acute conditions caused by sudden catastrophic events
- These patients may be registered on the palliative register in primary care. Deactivation should also be considered when patients have a Do Not Attempt Cardiopulmonary Resuscitation (DNCPAR) order in place. Maintaining an ICD/CRT-D in active defibrillation mode is necessarily inconsistent with a DNCPAR order. For example, some patients don’t want external cardiopulmonary resuscitation (CPR) but wish their ICD/CRT-D to be active for the treatment of dysrhythmia. Note that deactivation refers to the cessation of therapies for VT and VF. Any pacemaker function will generally continue.
Multidisciplinary Team Approach
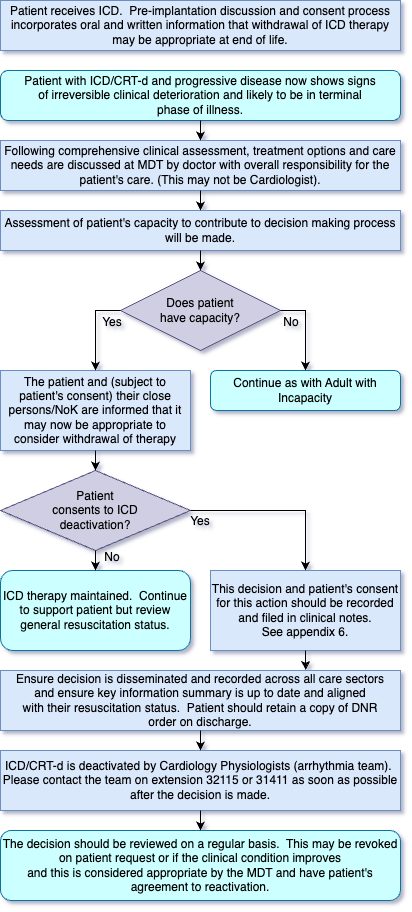
- It is essential that a comprehensive assessment of the patient is made prior to any decision regarding deactivation of ICD/CRT-D. This assessment may include a multidisciplinary team and should include the physician responsible for patient care (this could be Oncologist, GP, Cardiologist or other clinician), the patient and where possible a representative for the patient (e.g. relative). The patient’s autonomy and their wishes should be considered at all times and the decision around deactivation should be clearly documented. Patients with mental capacity have the legal and ethical right to request the withdrawal of medical interventions, including defibrillation therapy, which sustain life. Please see the NHS Scotland Do not attempt resuscitation (DNACPR) Adult Integrated Policy for more information (Scottish Government 2010).
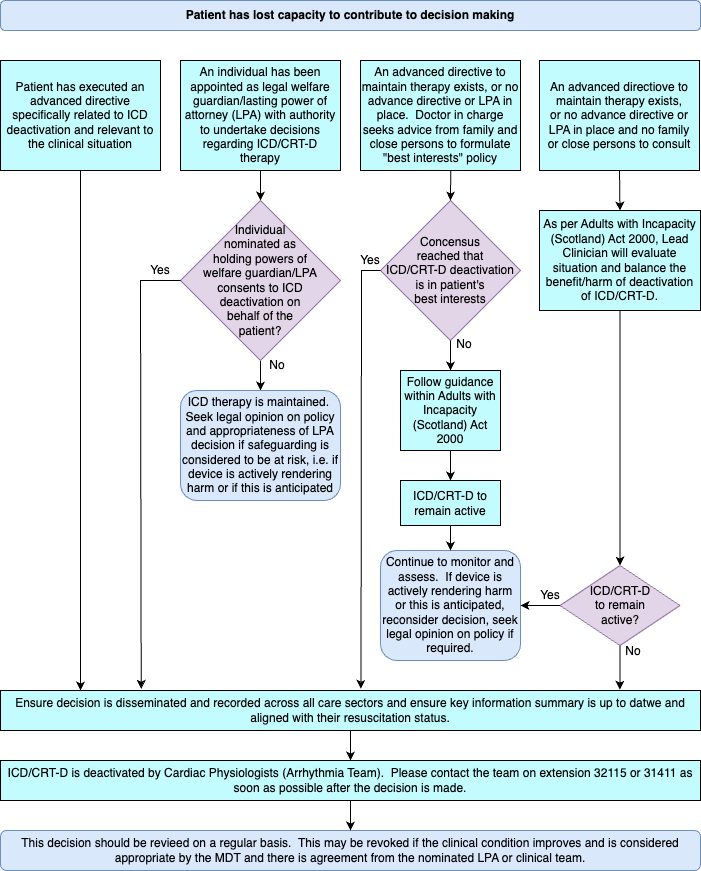
- Patients who are judged to lack capacity to make decisions about their care should be managed under the principles of the Adults with Incapacity (Scotland) Act 2000. Please contact the Dumfries and Galloway Arrhythmia Team (Cardiology Physiologists) on 01387 241429 (ext 32115 or 31411 from within the hospital) as soon as possible if device deactivation is being considered. A cardiac devices MDT is held once a month in Cardiology and where possible patients should be referred for discussion at this meeting. Please see algorithms one and two below for more advice about deactivation.
Summary
- Consider defibrillator deactivation for patients:
- In the last year of life
- On the palliative care register
- Receiving end of life care
- In whom a DNACPR order is in place
- Offer support and written guidance to patients and families and respect the patient’s decision.
- Let the Cardiology Team know as soon as possible when you are considering defibrillator deactivation
- 01387 241429 (ext 32115 or 31411 from within the hospital)
- [email protected]
- Senior clinician should document decision to deactivate defibrillator clearly, in writing, with date and time of decision and confirming patient’s consent.
- Click link here for full document, algorithms and appendices.
Appendix 1: ICD / CRT-D Functions
- Implantable Cardioverter Defibrillators (ICD) have a number of key functions:
- Automatic administration of defibrillation shocks to terminate Ventricular Fibrillation (VF) or fast Ventricular Tachycardia (VT)
- Basic pacing used for bradycardia
- Anti-tachycardia pacing (ATP) to terminate slower VT
- The basic pacemaker functions of the ICD will not be deactivated when the defibrillator therapy and ATP function is deactivated.
- Cardiac Resynchronisation Therapy with Defibrillator (CRT-D): this has the same functions as an ICD but also has the ability to coordinate/resynchronise cardiac contractility. The resynchronisation ability of this device would not be deactivated when the defibrillator therapy is deactivated. This should be made clear to patients during discussions around deactivation.
Appendix 2: Emergency deactivation
- Emergency deactivation can be achieved by secure placement of a doughnut or other specialist cardiology magnet externally on the chest, over the device. This is only a temporary measure and full deactivation should be undertaken as soon as practicable. Ideally cardiology physiologists are contacted as soon as deactivation is being considered. Doughnut magnets are held in ITU, Cardiology ward, the Emergency department and in Cardiology Outpatients.
- To contact the cardiac physiologists at the Device Clinic, please phone extension 32115 or 31411.
Appendix 3: Post Mortem Device handling
- When the patient dies, the device still needs to be fully interrogated (in case of arrhythmic death or Medical Device Alert) and deactivated by the cardiac physiologists from the Device Clinic before the body leaves the hospital (if hospital death). This will avoid the risk of electric shock to the mortuary technicians / undertakers. These specialist devices, including pacemakers, must be explanted prior to cremation of the body.
- To contact the cardiac physiologists at the Device Clinic, please phone extension 32115 or 31411.
Appendix 4: Cardiology Physiologist’s DNA-CPR Protocol
- When an ICD/CRT-D patient has a DNA-CPR form in their case notes and device deactivation has been discussed and agreed as appropriate, the following should be adhered to:
- Ensure that the appropriate consultant has informed cardiac physiologist to turn off device first (this should be documented in case notes).
- Review case notes to ascertain whether patient is aware of DNA-CPR.
- Turn off all defibrillator therapies (ATP, shock therapy and alerts). Do not turn off pacemaker/CRT function.
- Print out two copies of final settings, highlighting therapy off: keep one copy in ICD/CRT-D notes and other in patient case notes
- Write in case notes action performed and which consultant requested ICD/CRT-D to be programmed off.
N.B. If patient circumstances change (i.e. patient improves) and it is deemed appropriate to turn therapy back on, this should be done before patient leaves the hospital. Ward staff looking after patient should be made aware of this.
References
- Treatment and care towards end of life: good practice in decision making. London 2010 General Medical Council
- ICD deactivation at the end of life: Principles and practice. British Heart Foundation London 2013
- Do Not Attempt Resuscitation (DNACPR) Integrated Adult Policy- Decision making and Communication. Scottish Government Edinburgh 2010
- Appendix 6 – Form Consent for Deactivation of Implanted Cardioverter Defibrillator