Paediatric Diabetic Ketoacidosis (DKA) Guideline
For the BSPED DKA Management Integrated Care pathway please click on the link below and if the link is not working please print it out from the BSPED website:
https://www.bsped.org.uk/clinical-resources/bsped-dka-guidelines/
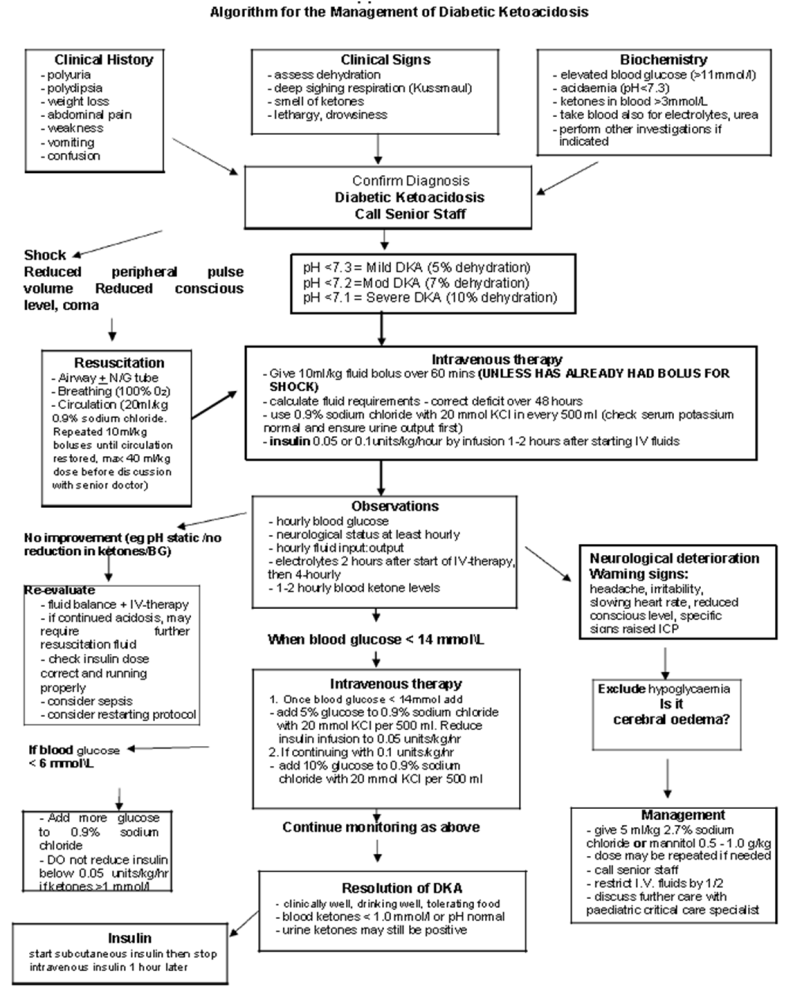
Detailed DKA management guidance is as below,
DKA is a medical emergency – Inform the Oncall paediatric consultant as soon as possible.
Where young people aged 16-18 years are managed by adult medical teams because of local arrangements it is considered appropriate for them to be managed using local adult guidelines that the teams are familiar with rather than using potentially unfamiliar paediatric guidelines.
Where individuals aged 16-18 are managed by our Paediatric team the Paediatric guidelines should be followed.
| DKA Definition Acidosis pH < 7.3 or Plasma Bicarbonate < 15mmol/l Ketonaemia Finger –Prick blood ketones > 3.0 mmol/l Blood Glucose > 11mmol/l (Could be normal in children with known diabetes) | Clinical Features of DKA: Acidotic respiration Dehydration Drowsiness Abdominal pain Vomiting |
- Mild DKA – venous pH 7.2- 7.29 and/or bicarbonate < 15 mmol/l. Assume 5% dehydration.
- Moderate DKA – venous pH 7.1-7.19 and/or bicarbonate < 10 mmol/l. Assume 7% dehydration.
- Severe DKA – venous pH less than 7.1 and/or bicarbonate < 5 mmol/l. Assume 10% dehydration.
A. Initial Management of DKA
- General Resuscitation: A, B, C
Airway: Ensure that the airway is patent and if the child is comatose, insert an airway.
If consciousness reduced or child has recurrent vomiting, insert N/G tube, aspirate and leave on open drainage.
Seek urgent anaesthetic review and discuss with a paediatric critical care specialist if the child or young person has a reduced level of consciousness and is unable to protect their airway.
Breathing: Give 100% oxygen by face-mask as needed.
Circulation: Insert 2 x IV cannulas and take blood samples (see below)
Cardiac monitor for T waves (peaked in hyperkalaemia)
Measure blood pressure and heart rate.
2. Initial Fluid Bolus:
a) Shocked patients require adequate fluid volume resuscitation. A fluid bolus of 20ml/kg may be indicated.
- Patients with shock require appropriate restoration of their circulation and circulatory volume. Shocked patientsshould receive a 20 ml/kg bolus of 0.9% saline over 15 minutes. Shock is defined by the APLS definition of tachycardia, prolonged central capillary refill, poor peripheral pulses and hypotension (though this is a late sign of shock). It is not just poor peripheral perfusion.
- Shocked patients will require high dependency care and should be discussed with the Consultant on-call paediatrician or Anaesthetist available at the earliest opportunity.
- Following the initial 20 ml/kg bolus shocked patients should be reassessed and further boluses of 10 ml/kg may be given if required to restore adequate circulation up to a total of 40 ml/kg at which stage inotropes should be considered.
- Whilst excessive fluid should be avoided because of the risk of cerebral oedema it is important to ensure that the circulation is adequate and fluid should be given to support this.
b) All children and young people with mild, moderate or severe DKA who are not shocked and are felt to require IV fluids should receive a 10 ml/kg 0.9% sodium chloride bolus over 60 minutes.
3. Investigations:
Blood glucose
FBC
Urea and electrolytes, CRP
Blood Gases (Venous or Capillary)
Ketones – Near patient blood ketones (beta – hydroxybutyrate)
+/- other investigations only if indicated e.g. CXR, CSF, throat swab, blood culture, urinalysis, culture and sensitivity etc.
In addition for ALL new diabetes patients –
- Thyroid function tests including thyroid peroxidise antibodies
- Islet Cell Antibodies (Anti GAD, Anti-IA2 antibodies)
- TTG (Tissue Transglutaminase) Coeliac screening
Management of DKA
1. Clinical Assessment (Medical & Nursing)
- ALL children with DKA are high-dependency patients and require a high level of nursing care, even if on general paediatric wards.
2. Conscious Level – Institute hourly neurological observations including Glasgow Coma Score whether or not drowsy on admission.
If reduced conscious level on admission, or there is any subsequent deterioration
- Seek urgent anaesthetic help if airway cannot be protected
- discuss with the responsible consultant paediatrician on-call
- consider transfer to PICU/HDU if available
- consider instituting cerebral oedema management (discuss with PICU Consultant)
Conscious level is directly related to degree of acidosis, but signs of raised intracranial pressure suggest cerebral oedema – initiate cerebral oedema management.
3. Full Examination – looking particularly for evidence of –
- Cerebral oedema (headache, irritability, slowing pulse, rising blood pressure, reducing conscious level. Papilloedema is a late sign)
- Infection
- Ileus
WEIGH THE CHILD – If this is not possible because of the clinical condition, use the most recent clinic weight as guidance or an estimated weight accordingly.
4. Consider PICU or HDU for the following, and discuss with a PICU consultant
- severe acidosis pH<7.1 with marked hyperventilation
- severe dehydration with shock
- depressed sensorium with risk of aspiration from vomiting
- very young (under 2 years)
- Signs and symptoms suggestive of Cerebral Oedema
5. Nursing Observations to be carried out
Ensure full instructions are given to the senior nursing staff emphasising the need for:
- strict fluid balance
- measurement of volume of every urine sample
- hourly capillary blood glucose measurements
- capillary blood ketonelevels every 1-2 hours
- blood ketones testing
- half- hourly to hourly neurological observations initially
- hourly BP and basic observations
- twice daily weight; can be helpful in assessing fluid balance
- reporting immediately to the medical staff, even at night, symptoms of headache, or slowing of pulse rate, or increased BP, or any change in either conscious level or behaviour
- reporting any changes in the ECG trace, especially T wave changes suggesting hyper- or hypokalaemia
2. Management of Fluids:
N.B. It is essential that all fluids given are documented carefully, particularly the fluid which is given in A&E/Casualty and on the way to the ward, as this is where most mistakes occur.
Volume of Fluid:
Children with shock should have been adequately resuscitated with appropriate fluid volume replacement. Other patients with DKA will have received an initial fluid bolus of 10ml/kg as part of the routine management of DKA.
Requirement = Deficit + Maintenance
1) Fluid Deficit: Estimation of the fluid deficit should be based on the initial blood pH. The fluid deficit should be replaced over 48 hours alongside maintenance fluids.
| -Assume a 5% fluid deficit in children and young people in mild DKA (indicated by a blood pH 7.2-7.29 &/or bicarbonate <15) -Assume a 7% fluid deficit in children and young people in moderate DKA (indicated by a blood pH of 7.1- 7.19 &/or bicarbonate <10) -Assume a 10% fluid deficit in children and young people in severe DKA (indicated by a blood pH <7.1 &/or bicarbonate <5) |
2) Maintenance: Calculate the maintenance fluid requirement using the traditional method of calculations as below,
- 100 ml/kg/day for the first 10 kg of body weight
- 50 ml/kg/day for the next 10 to 20 kg
- 20 ml/kg/day for each additional kilogram above 20 kg
N.B. Neonatal DKA will require special consideration and larger volumes of fluid than those quoted may be required, usually 100-150 ml/kg/24 hours
3) Resuscitation fluid
- The volume of any fluid boluses given for resuscitation in children with shock should NOT be subtracted from the estimated fluid deficit.
- The initial 10ml/kg bolus given to all non-shocked DKA patients requiring IV fluids SHOULD be subtracted from total calculated fluid deficit.
Fluid Calculation
Calculate the fluid deficit (either 5%, 7% or 10% dehydration depending on whether the patient has mild, moderate or severe DKA), subtract the initial 10ml/kg bolus then divide this over 48 hours and add to the hourly rate of maintenance fluid volume , giving the total volume evenly over the next 48 hours. i.e.
Hourly rate = ({Deficit – initial bolus} / 48hr) + Maintenance per hour
https://www.dka-calculator.co.uk/ – Please use DKA calculator if needed.
Weight – Wherever possible the patient’s actual weight on admission should be used rather than an estimated weight or approximation. To avoid excessive amounts of fluid in overweight and obese children it is recommended that consideration be given to using a maximum weight of 80kg or 98th centile weight for age (whichever is lower) when calculating both deficit and maintenance requirements.
Examples :
a) A 20 kg 6 year old boy who has a pH of 7.15 (Moderate DKA => 7% Dehydrated) will receive a 10ml/kg bolus (200mls fluid) over 60 minutes as part of his initial management. His ongoing fluids will comprise:
Deficit 7% x 20kg = 1400 ml
Subtract initial bolus = 1400 – 200 = 1200 ml to be replaced over 48 hours
= 25 ml/hr
Maintenance = 1500 ml per day total for 20kg (over 24 hours)
= 62 ml/hr
Total Fluid = 25 ml/hr + 62 ml/hr
= 87 ml/hr
b) A 60 kg 15 year old girl with a pH of 6.9 who was shocked at presentation has received 30ml/kg of 0.9% Saline for resuscitation. These boluses are not subtracted from ongoing maintenance fluids. Her ongoing fluids will comprise:
Deficit 10% x 60kg = 6000 ml to be replaced over 48 hours
= 125 ml/hr
Maintenance = 2300 ml per day total for 60kg (over 24 hours)
= 96 ml/hr
Total Fluid = 125 ml/hr + 96 ml/hr
= 221 ml/hr
Do not give additional intravenous fluid to replace urinary losses. Urinary catheterisation should be avoided but may be useful in the child with impaired consciousness.
7. Potassium
Ensure that all fluids (except any initial boluses given) contain 40 mmol/l potassium chloride, unless there is evidence of renal failure. Hypokalaemia can occur up to 48 hours after starting DKA treatment.
Potassium levels in the blood will fall once insulin is commenced.
Therefore ensure that every 500 ml bag of fluid contains 20 mmol KCl (40 mmol per litre).
Check U & E’s & CBG 2 hours after resuscitation is begun and then at least 4 hourly and alter potassium replacements accordingly. Use cardiac monitoring.
If the child or young person with DKA develops hypokalaemia (potassium below 3 mmol/litre):
- think about further reducing the insulin infusion
- discuss urgently with Consultant On Call/Anaesthetist, because a central venous catheter is needed for intravenous administration of potassium solutions above 40 mmol/litre.
8. Insulin
Once rehydration fluids and potassium are running, blood glucose levels will start to fall. There is some evidence that cerebral oedema is more likely if insulin is started early. Do not give bolus doses of intravenous insulin.
| Therefore start an intravenous insulin infusion 1-2 hours after beginning intravenous fluid therapy |
Make up a solution of 1 unit per ml. of human soluble insulin (e.g. Actrapid) by adding 50 units (0.5 ml) insulin to 49.5 ml 0.9% saline in a syringe pump. Attach this using a Y-connector to the IV fluids already running. Do not add insulin directly to the fluid bags.
Use the soluble insulin infusion at a dosage between 0.05 and 0.1 units/kg/hour.
An infusion rate of 0.05 Units/kg/hr is likely to be sufficient in most cases though in severe DKA an infusion rate of 0.1 Units/kg/hr may be needed.
Please check with your Consultant OnCall on what dosage to start.
For children and young people on continuous subcutaneous insulin infusion (CSII) pump therapy, stop the pump when starting intravenous insulin.
For children on MDI, you may wish to consider continuing the long acting insulin at the same dose and at their usual time during their DKA management.
9. Bicarbonate
Do not give intravenous sodium bicarbonate to children and young people with DKA.
Only consider bicarbonate if there is life threatening hyperkalaemia or in severe acidosis with impaired myocardial contractility. It is anticipated that this would only ever be done following discussion with an Intensivist.
10. Risk of Venous Thrombosis
Be aware that there is a significant risk of femoral vein thrombosis in young and very sick children with DKA who have femoral lines inserted. Line should be in situ as short a time as possible. Thromboembolic prophylaxis should be considered in young people >16 years (in line with NICE guidance), in young women taking the combined oral contraceptive pill and sick patients with femoral lines, following discussion with an Intensive Care Specialist.
C. Continuing Management = Fluid/Insulin
Continue with 0.9% sodium chloride containing 20 mmol potassium chloride in 500ml until blood glucose levels have fallen below 14 mmol/l.
If the blood glucose rises out of control, or the pH level is not improving after 4-6 hours consult senior medical staff and re-evaluate (possible sepsis, insulin errors or other condition), and consider starting the whole protocol again.
If the blood ketone level is not falling within 6–8 hours review patient, check IV cannua for insulin delivery issues etc. Think of increasing the insulin dosage to 0.1 units/kg/hour or greater as appropriate.
| Once the blood glucose has fallen below 14 mmol/l add glucose to the fluid and think about the insulin infusion rate, as follows – If ketone levels are less than 3 mmol/l – change the fluid to 0.9% NaCl with 5% glucose and 20 mmol KCl per 500ml . – reduce to or maintain at an insulin infusion rate of 0.05 units/kg/hr If ketone levels are above 3 mmol/l – change to 0.9% NaCl with 10% glucose and 20 mmol KCl per 500ml, in order to prevent hypoglycaemia when the higher dose of insulin is continued – maintain the insulin infusion rate at 0.05 to 0.1 units/kg/hour to switch off ketogenesis |
DO NOT stop the insulin infusion while glucose is being infused, as insulin is required to switch off ketone production.
If the blood glucose falls below 6 mmol/l
- increase the glucose concentration of the intravenous fluid infusion, and if there is persisting ketosis, continue to give insulin at a dosage of least 0.05 units/kg/hour
If the blood glucose falls below 4 mmol/l
- give a bolus of 2 ml/kg of 10% glucose and increase the glucose concentration of the infusion. Insulin can temporarily be reduced for 1 hour.
If acidosis is not correcting, consider the following
- insufficient insulin to switch off ketones
- inadequate resuscitation
- sepsis
- hyperchloraemic acidosis
- salicylate or other prescription or recreational drugs
Once all these causes of acidosis have been excluded, and if ketones are falling gradually, then residual acidosis is likely to be due to hyperchloraemia, and this can be left to resolve on its own, and does not require any treatment.
Insulin management once ketoacidosis resolved
Continue with IV fluids until the child is drinking well and able to tolerate oral fluids.
| Only change to subcutaneous insulin once blood ketone levels are below 1.0 mmol/l or pH is normal. For a child or young person who is newly diagnosed or those who are already on Basal Bolus regimen, start subcutaneous insulin at least 30 minutes before stopping intravenous insulin. Preferably plan to start this before a main meal along with the background insulin. For a child or young person with DKA who is using insulin pump therapy, restart the pump at least 60 minutes before stopping intravenous insulin. Change the insulin cartridge and infusions set, and insert the cannula into a new subcutaneous site. |
D. How to make up special fluids
- 500ml bag of 0.9% sodium chloride and 5% glucose containing 20 mmol potassium chloride
- Remove 50ml from a bag of Sodium Chloride 0.9% with 20mmol KCL in 500ml
- Draw up 50ml of Glucose 50% using a syringe and add to the above bag which will make the Glucose concentration 5%
- Mix well before administration
- 500ml bag of 0.9% Sodium chloride and 10% glucose containing 20mmol potassium chloride
- Remove 50ml from a bag of Glucose 5% & Sodium Chloride 0.9% with 20mmol KCL in 500ml
- Draw up 50ml of Glucose 50%using a syringe and add to the above bag which will increase the Glucose concentration to 10%
- Mix well before administration
E. Management of Cerebral Oedema
The early signs and symptoms of cerebral oedema include:
- headache
- agitation or irritability
- unexpected fall in heart rate
- increased blood pressure
- specific neurological signs (eg. cranial nerve palsies)
- abnormal posturing
- Pupillary inequality or dilatation
- abnormal breathing pattern
If cerebral oedema is suspected inform the Consultant on call immediately
| If cerebral oedema is suspected in these children or young people, treat immediately with the most readily available of Hypertonic saline 2.7% or 3% – (2.5-5 ml/kg over 10-15 minutes) or Mannitol 20% (0.5-1 g/kg over 10-15 minutes). In addition fluids should be restricted to ½ maintenance rates. The child will need to be moved to PICU. Do not intubate and ventilate until an experienced doctor is available. Once the child is stable, exclude other diagnoses by CT scan. The effect of mannitol should be apparent within 15 minutes and typically lasts for 120 minutes. If there is no improvement with mannitol within 30 minutes a repeated dose of mannitol may be given (or hypertonic saline may be preferred). Mannitol may promote a brisk diuresis due to its osmotic effect and renal excretion. If mannitol was given initially and there is no response to mannitol treatment within 15-30 minutes then hypertonic saline may be also be given and there is some suggestion that the effect of mannitol and hypertonic saline may be additive. |