Warning: Undefined variable $nameCategory in /home/docthand/public_html/wp-content/themes/docthand/single-post_handbook.php on line 42
Warning: Attempt to read property "term_id" on null in /home/docthand/public_html/wp-content/themes/docthand/single-post_handbook.php on line 42
Assessment & Management of Acute Pain
This guide is specifically for Acute ‘Nociceptive’ Pain that is not resulting from cancer.
Our Analgesic Ladder represents initial safe starting drugs and doses in acute pain.
Pain can be categorised into the following:
We advocate the following steps in before prescribing Analgesia:
Step 3 – Prescribe Analgesia (See Analgesic Ladder)
Step 4 – Anticipate and Manage the Opioid Side-effects
Step 6 – Prepare for the Analgesic Plan on Discharge from Hospital
Step 1: Assessment of Pain
History – Questions not to forget
Presenting complaint:
- What does the pain feel like (e.g. ‘aching’, ‘burning’, ‘throbbing’, ‘stabbing’)?
- What is the effect on physical function?
- Can they cough?
- Can they deep breathe?
- Can they get out of bed or reposition in bed?
- Can they sleep?
Drug History:
- What is the current analgesic strategy? What has helped/not helped so far?
- Was the patient taking opioids or other analgesics pre-hospital? Has this been considered in their current prescription?
Assessment of Severity:
- Assessment of severity is important because it:
- Helps guide initial choice of treatment
- Helps to measure response to treatment
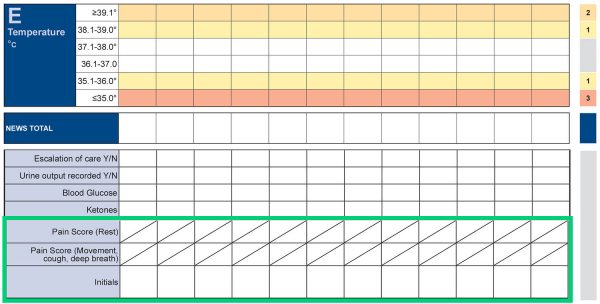
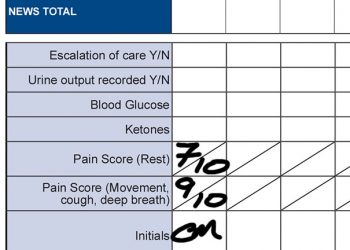
- We recommend that you choose one of the following pain assessment tools. Remember pain should be assessed together with the NEWS observation at rest AND on movement (e.g. deep breathing/coughing/repositioning):
- The Verbal Rating Scale should be used in patients who can understand the use of the tool and verbalise their pain. (e.g. 0 to 10)
- A 4-point Categorical Rating Scale (none, mild, moderate, severe) should be used in patients who can understand the use of the tool and verbalise their pain, but may not understand the VRS. (e.g. none, mild, moderate or severe)
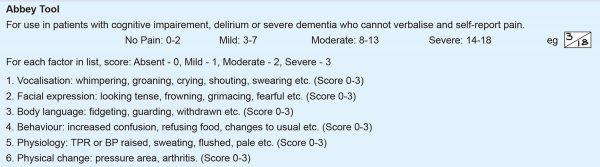
- The Abbey Pain Assessment Tool should be used in patients who have cognitive impairment and/or are unable to verbalise their pain. There is a section on the NEWS chart to guide you in the use of this. (See below). Also available on MDCalc.com – Abbey Pain Scale.
Document the Severity
Any member of medical, nursing or allied-health professional staff can assess pain using one of the above tools. It is important that the severity score is documented appropriately on the NEWS chart. See below.
Step 2 – Categorise Pain
“Not all pain is the same”.
- It is important to classify the pain (make a pain diagnosis) because this helps us to choose the best treatment.
- Pain can be classified in many ways, but it is helpful to classify pain using three main questions:
- How long has the patient had pain?
- What is the cause?
- What is the pain mechanism?
Acute versus chronic pain (duration)
- Pain can be acute (pain for less than 3 months) or chronic (pain for more than 3 months or pain persisting after an injury heals). Sometimes, a patient with chronic pain may experience additional acute pain (acute on chronic pain). NB: This guideline is targeted at Acute pain and Acute-on-chronic pain only.
Cancer versus non-cancer pain (cause)
Cancer pain
NB: This guideline is targeted at Non-cancer pain. If you think your patient has Cancer-related pain, then you may wish to refer to the Scottish Palliative Care Guidelines or contact the in-hospital Palliative Care Team.
-
- Scottish Palliative Care Guidelines
- Palliative Care Team: (contacted through switchboard)
Non-cancer pain
- There are many different causes, including:
- Surgery or injury
- Surgical pathology (e.g. appendicitis, pancreatitis)
- Degenerative disease (e.g. arthritis)
- Childbirth
- Nerve compression or injury (e.g. sciatica, neuralgia)
- Pain may be acute and last for a limited time or may become chronic.
- The cause may or may not be obvious.
Nociceptive versus neuropathic pain (mechanism)
Pain can also be classified by mechanism (the physiological or pathological way the pain is produced). The pain can either be nociceptive, neuropathic or mixed (both nociceptive and neuropathic).
Nociceptive pain
- Commonest type of pain following tissue injury.
- Sometimes called physiological or inflammatory pain.
- Caused by stimulation of pain receptors in the tissues that have been injured.
- Has a protective function.
- Patients describe pain as sharp, throbbing or aching, and it is usually well localised (the patient is able to point to exactly where the pain is).
- Examples: Pain due to a fracture, appendicitis, burn.
Neuropathic pain
- Caused by a lesion or disease of the sensory nervous system.
- Sometimes called pathological pain.
- Tissue injury may not be obvious.
- Does not have a protective function.
- Patients describe neuropathic pain as ‘burning’ or ‘shooting’. They may also complain of numbness or pins and needles. The pain is often not well localised.
- Examples: Post-amputation pain, pain associated with diabetes, sciatica.
NB: This guideline is targeted at Nociceptive pain. If you think your patient has Neuropathic pain, then you may wish to refer to the Acute Pain Team. Alternatively, there is an Algorithm for Management of Neuropathic Pain available on the NHSD&G Adult Joint Formulary 2022.
Step 3: Prescribe Analgesics
- If after Step 1 and Step 2 you are sure you are treating acute (or acute-on-chronic), nociceptive, non-cancer pain, then please refer to the Analgesic Ladder. This represents initial safe starting drugs and doses in acute pain.
- Before using this ladder, you need the following information:
- Is the oral route available?
- Patient’s Weight.
- Is your patient in a ‘Special Group’: Renal or Hepatic Impairment, Poor Nutritional Status; Frailty; Opioid use disorder, Chronic Pain.
NB: patients with a history of either chronic pain or chronic opioid analgesics may need either higher doses of opioid analgesics or alternative analgesics. For complex patients such as these, please seek help from the Acute Pain Team.
Analgesic Ladder for Adults in Acute Pain
(see mild pain protocol on HEPMA) |
|
| - Oral Paracetamol 1g regularly four times a day ( 500mg four times a day if <50kg or in hepatic impairment/nutritional deficiency) - ± 3 days of Oral Ibuprofen 400mg three times a day (check for contraindications) | - IV Paracetamol 1g regularly four times a day (500mg four times a day if <50kg or hepatic impairment/nutritional deficiency) |
(see moderate pain protocol on HEPMA) |
|
| - Oral Paracetamol 1g 500mg four times-a-day if <50kg or hepatic impairment/nutritional deficiency) - Oramorph: 5mg five times-a-day + hourly PRN (2.5mg five times-a-day if elderly) - ± 3 days of Oral Ibuprofen 400mg three times-a-day (check for contraindications) If renal impairment change Morphine to: - Oxynorm 2.5mg five times-a-day + hourly PRN (1.25mg five times-a-day if elderly) | -IV Paracetamol 1g four times-a-day (500mg four times-a -day if <50kg or hepatic impairment/nutritional deficiency) -Subcutaneous Morphine 2.5mg five times-a-day + hourly PRN (1.25mg five times-a-day if elderly) If renal impairment change Morphine to: - Subcutaneous Oxynorm 1.25mg five times-a-day + hourly PRN (0.675mg five times-a-day if elderly) |
(see severe pain protocol on HEPMA) |
|
| - Regular Paracetamol +/- Ibuprofen (see above) If no oral route IV Diclofenac 75mg twice daily can be used (check for contraindications and d/w Acute Pain Team. Diclofenac is given as an IV infusion). - Titrate: IV Fentanyl or Morphine (avoid Morphine in renal impairment) - Intravenous PCA: Protocol E-Fentanyl OR Protocol A-Morphine (avoid Morphine in renal impairment) Please seek advice from pain team before modifying the bolus dose or background rate on a PCA. - If unable to control pain using this regime then please call the Acute Pain team |
|
- We recommend that the prescription is reviewed daily in accordance with pain assessment. The prescription should be de-escalated as soon as it is clinically indicated to do so and a clear deprescribing plan for opioids should be in place at the time of discharge from hospital.
- Please note the following additional resources that should be consulted when indicated:
- Renal Handbook
- Use MUST/Refeeding Score to identify nutritional deficiency
Step 4: Management of the Side Effects of Opioids
Constipation
-
- Within the BNF, there is a helpful treatment summary on Constipation which the authors of this guideline encourage you to refer to. Important points to highlight include:
- Opioid-induced constipation (OIC) is a common side effect of opioids and thus treatment for this should begin with the commencement of opioids. Treatments for OIC include:
- Non-pharmacological – Increase in dietary fibre, increase in oral fluid intake, increase in physical activity.
- Pharmacological – Laxatives
- Before prescribing laxatives, make sure that the patient is constipated due to opioids and that it is not secondary to an underlying undiagnosed complaint.
- Contraindications to laxatives include: intestinal obstruction, intestinal perforation, paralytic ileus and inflammatory conditions of the intestinal tract.
- In patients with opioid-induced constipation, an osmotic laxative and a stimulant laxative are recommended. Bulk-forming laxatives should be avoided.
- Within the BNF, there is a helpful treatment summary on Constipation which the authors of this guideline encourage you to refer to. Important points to highlight include:
NB: This does not apply to patients on the Enhanced Recovery after Surgery (ERAS) pathway. Please seek advice from the surgical team before prescribing laxatives for ERAS patients.
Nausea
Patients receiving regular opioids should be prescribe a PRN anti-emetic in anticipation of this common side effect. First line agents are Ondansetron and Cyclizine. NB: Constipation is a common side effect of ondansetron.
Respiratory Depression
Respiratory depression is a much-feared but thankfully rare harm associated with the use of opioids. However, fear of this side effect must not prevent the patient receiving adequate analgesia.
To reduce the risk of harm from respiratory depression, we recommend awareness of the following points:
- Choice of appropriate analgesic in at-risk patients, such as Renal Impairment, as per the Analgesic Ladder.
- Deepening levels of sedation usually precede respiratory depression and should be a trigger for suspending opioids pending further assessment.
- A Respiratory Rate of <12/minute in a patient who is not physiologically asleep is highly sensitive of opioid overdose, especially if constricted pupils or stupor are present
- Naloxone is the antidote to opioids. For guidance on how to safely administer Naloxone, please refer to our Flowchart for Intravenous Opioids
Step 5: Reassess Pain
- We recommend pain be reviewed at least daily by the Parent Team.
- Assess the patient. Are they still in acute pain?
- What is the severity of their pain in each of the following:
- at rest
- on deep breathing
- with coughing/movement?
| Category | VRS | CRS | APAT |
|---|---|---|---|
| Mild Pain | 0-3 | 'Mild Pain' | 3-7 |
| Moderate Pain | 4-6 | 'Moderate Pain' | 8-13 |
| Severe Pain | 7-10 | 'Severe Pain' | ≥14 |
VRS=Verbal Rating Scale, CRS= Categorical Rating Scale, APAT=Abbey Pain Assessment Tool
| Has the pain severity improved from their previous documented severity category? |
|---|
| If ‘Yes’ in all three of the above - DE-ESCALATE the prescription -Move to the lower rung in the analgesic ladder whilst continuing PRN opioids |
| If ‘No’ in any of the above three - ESCALATE the prescription. Consider the following: - If new severe pain, refer to the Analgesic Ladder for the Management of Severe Pain (above). - Does the patient require IV titration to manage acute severe pain? If so, refer to Administration of IV Opioids Flowchart. Or, if requiring >2 doses of PRN analgesia per 24hr period, consider the following: - Increasing the regular and PRN oral opioid dose by 50-100% - Stopping the regular and PRN immediate-release oral opioid and prescribing a long-acting opioid* |
Long-acting oral opioids should not be prescribed in patients with post-operative paralytic ileus. They should be used in caution in patients with AKI/CKD and hepatic impairment.
NB Pain that is not responding tro treastment may be a sinister sign of missed pathology. Have a low threshold for seeking senior review if you are concerned about this.
It is also important to taper or stop the opioid regimen if:
-
- the underlying painful condition resolves
- opioid medication is not providing useful pain relief.
- the patient develops intolerable side effects
Increasing opioid load above 90mg oral morphine equivalent/24hours dose is unlikely to yield further benefits but exposes the patient to increased harm.
Step 6: Discharge from Hospital
- On discharge from hospital, the discharge letter must include accurate details of all analgesia provided.
- The prescription of any opioid analgesia for use post-discharge must include a de-prescribing plan.
Paracetamol – Important Points
Paracetamol should be used with caution in cases of:
- hepatocellular insufficiency
- severe renal insufficiency (please refer to the Renal Handbook via the Clinical Handbook page on Beacon)
- chronic alcoholism
- chronic malnutrition (low reserves of hepatic glutathione)
- dehydration
Safe Dosing of Paracetamol
| Patient Weight | Dose per Administration | Maximum Dose in 24 Hours |
|---|---|---|
| 33-50kg | 15mg/kg | 60mg/kg *not exceeding 3g |
| >50kg and additional risk factors for hepatotoxicity | 1g | 3g |
| >50kg and no risk factors for hepatotoxicity | 1g | 4g |
| (extrapolated from the SmPC (https://www.medicines.org.uk/emc/) Accessed 28/6/22 | ||
NSAIDs – Important Points
- Check for contra-indications to Non-Steroidal Anti-Inflammatory Drugs before prescribing them
- Consider Renal, Cardiac and Hepatic impairment,
- Suspected/high risk of haemorrhage,
- coagulation abnormalities,
- hypersensitivity to aspirin,
- previous/active peptic ulceration etc.
Links
- Administration of IV Fentanyl & Morphine for Management of Acute Severe Pain in Adults
- IV Fentanyl & Morphine for Acute Pain in Adults [pdf]
- Analgesic Ladder for Acute Pain [pdf]
Content by Duncan Thomson, Libby Jardine, Alasdair Hay