In this section : Gastrointestinal
Coeliac diagnosis pathway (Adults)
Sengstaken/Minnesota Tube for Bleeding Varices
Eradication of Helicobacter pylori
Acute Severe Ulcerative Colitis
Acute Upper GI Bleeding (AUGIB)
Iron Deficiency Anaemia
Dyspepsia
Nutritional Support in Adults
Refeeding Syndrome
Parenteral Nutrition
Crohn’s Disease
Acute Pancreatitis
Suspected Variceal Bleeding
Lower Gastrointestinal Bleeding
Home | Articles | Gastrointestinal |
Acute Pancreatitis
Last updated 4th March 2024
Causes
- Gallstones including microlithiasis and biliary sludge.
- Alcohol, though admission to hospital may represent an exacerbation of chronic pancreatitis rather than true recurrent acute pancreatitis.
- All other causes less common including hypertriglyceridaemia, hyperparathyroidism, pancreatic cancer, ERCP, trauma.
Presentation
- Epigastric pain is cardinal symptom, often radiating to back. Typically increases in severity over a few hours before reaching a plateau that may last for several days.
- Nausea and vomiting usually associated.
- Signs vary from mild tenderness to generalised peritonitis. Blue/grey discolouration of flanks (Grey-Turner’s sign) or in peri-umbilical area (Cullen’s sign) are features of pancreatic necrosis, and extremely bad prognostic signs.
- Severe acute pancreatitis may lead to multi organ failure.
- Painless acute pancreatitis is also recognised. Consider in shocked patient when no other cause apparent.
Diagnosis
- Requires typical features plus rise then fall of serum amylase.
- Most cases will have serum amylase > 300 (3 x ULN).
- Hyperamalysaemia also found in several non pancreatic diseases eg visceral perforation, small bowel obstruction, bowel ischaemia, leaking aortic aneurysm.
- Late presentations may require CT scan for diagnosis as amylase may have returned to normal.
- Also consider CT in shocked patient with no other apparent cause to rule out pancreatitis
Features That May Indicate A Severe Attack
- Clinical impression eg haemodynamic instability, low SpO2 etc
- Glasgow score 3 or more
- CRP > 200 mg/l
- Progressive organ failure
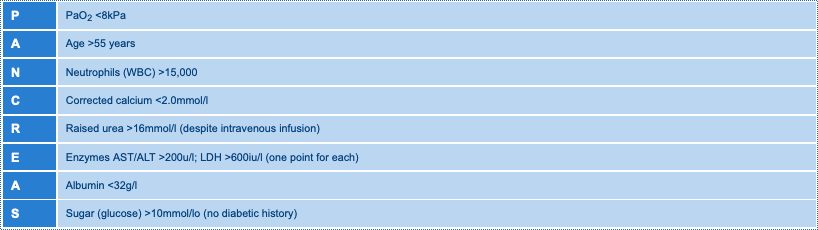
Glasgow Prognostic Score
- 3 or more of the following indicates severe acute pancreatitis (SAP):
Imaging
- CXR and AXR may give clues to the cause eg calcified gallstones, detect prognostic signs eg pleural effusion, or show complications eg localised ileus.
- Ultrasound is recommended as the initial investigation in all patients to show gallstones and dilated bile ducts, but is usually unhelpful for assessing pancreas.
- Main indication for CT is to detect and stage complications of SAP esp. pancreatic necrosis, the full extent of which cannot be appreciated until at least 3 days after onset of symptoms.
Initial Management
- Assess using ABCD approach.
- 80% cases have mild acute pancreatitis with low mortality (< 5%) and can be managed on a general ward.
- 20% cases have or develop SAP & will require care on HDU/ITU.
- Give high volume fluids – may need > 6 litres/24 hours in SAP (treat as retroperitoneal burns!)
- Give high flow oxygen pending blood gases.
- Catheterise to monitor urine output.
- Control pain with opiates – Refer to Assessment and Management of Acute Pain.
- NG tube not needed routinely but may be helpful if protracted vomiting occurs in the presence of a radiological ileus.
Nutritional Support
- Nutritional support is essential in patients with SAP.
- Attempt enteral route in all patients but when this is not tolerated additional or total parenteral nutrition may be needed.
- Nasogastric feeding has recently been shown to be as effective as naso-jejunal feeding.
Antibiotic Therapy
- Antibiotic prophylaxis has not been shown to reduce the risk of developing infected pancreatic necrosis.
- Antibiotics are indicated for
- Ascending cholangitis.
- Features of sepsis syndrome.
- SAP causing multi organ failure or pancreatic necrosis.
- Tazocin is antibiotic of choice for ascending cholangitis while Meropenem is best for SAP causing multi organ failure or pancreatic necrosis, given for 14 days.
Management of Gallstones
- ERCP and endoscopic sphincterotomy within 72 hours of symptom onset now recommended for patients with acute severe gallstone pancreatitis.
- Patients with mild gallstone pancreatitis should have cholecystectomy with intra-operative cholangiography, ideally during the same admission.
- For patients with severe gallstone pancreatitis, cholecystectomy may be delayed until systemic complications have resolved.
- For those unfit for cholecystectomy, endoscopic sphincterotomy alone may be sufficient treatment.
Pancreatic Necrosis
- Important to differentiate between sterile and infected pancreatic necrosis.
- Patients with > 30% necrosis on CT who are ill with falling CRP on Meropenem should continue with medical therapy but will require weekly CT to monitor.
- Patients with > 30% necrosis on CT who are unwell with rising CRP or definite signs of infected necrosis on serial CT should be discussed with Glasgow or Edinburgh Hepatobiliary Units for possible surgical necrosectomy.