In this section : Cardiac
Deactivation of Implantable Cardioverter Defibrillator
Extravasation of IV Amiodarone
Anticoagulation for AF, DVT and PE
Patients Returning from Interventional Cardiac Procedure
Cardiology Referrals
STEMI Thrombolysis Protocol
STEMI
Hypertensive Emergencies
Rate Control in AF
Heart Failure
Aortic Dissection
Non ST Elevation MI (NSTEMI)
Suspected Acute Coronary Syndrome
Pericardiocentesis
Pacemakers
Indications for Echocardiography
Bradycardia
Narrow Complex Tachycardia
Anti-Platelet Therapy in Coronary Heart Disease
Management of Acute AF
Rhythm Control in AF
Atrial Fibrillation
Hypertension
Ventricular Tachycardia
Cardiogenic Shock Complicating Acute Coronary Syndrome
Telemetry
Non ST Elevation MI (NSTEMI)
Last updated 8th December 2023
Definition of Myocardial Infarction
- MI currently defined by NICE as “evidence of myocardial necrosis in a clinical setting consistent with myocardial ischaemia”
- Type 1 MI is a primary coronary event due to plaque erosion and/or rupture
- Type 2 MI is secondary to ischaemia due to some other cause eg coronary spasm, anaemia, arrhythmia, hypertension or hypotension
- The main clinical definition requires a rise and/or fall of cardiac biomarkers, preferably troponin, with at least one value above the 99th centile of the upper reference limit (TnT ≥14ng/L in Dumfries) AND at least one of:
- Symptoms of ischaemia
- Resting ECG showing new ST-T changes or new LBBB
- Development of new pathological Q waves in the ECG
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
- It follows from the above that a normal ECG does not exclude MI
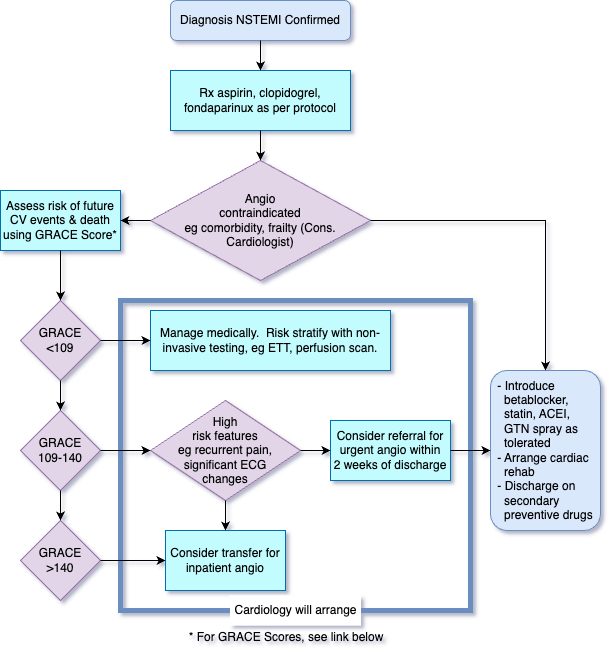
Risk Stratify with GRACE score
- GRACE >140: High risk: Should be considered for IP angiography
- GRACE 109-140: Intermediate risk. IP angiography should be considered if any high risk clinical features eg recurrent ischaemia, significant ECG changes. If no high risk clinical features present then consider referral for urgent OP angiography (will be performed within 2 weeks of discharge)
- GRACE <109. Low risk. Manage medically and perform risk stratification with non invasive ischaemia testing eg ETT, perfusion scan.
Caveats when using GRACE Score
- GRACE score is age dependent and thus disadvantages young NSTEMI patients. This should be considered when deciding on management of intermediate risk patients.
- Risk is dynamic and recurrent ischaemia should be an indication for IP angio even if presenting GRACE score was low to intermediate.
- Obvious Type 2 MI do not routinely need invasive angiography
- Sometimes frailty and co-morbidity mean angiography is not appropriate despite high GRACE score presentation.
Initial Management – If Not Taking DOAC or Warfarin
- Start immediate treatment with aspirin 300mg stat then 75mg daily, clopidogrel 300mg stat then 75mg daily.
- Start fondaparinux 2.5mg SC od. If CrCl <20ml/min switch to enoxaparin 1mg/kg SC od.
- Offer morphine 2.5-10mg IV with anti-emetic eg metoclopramide 10mg IV for pain
- Give oxygen but only if hypoxaemic
- Consider oral beta blocker if not bradycardic or hypotensive and not asthmatic eg atenolol 25mg, bisoprolol 2.5mg, metoprolol 50mg initially.
- Ensure on continuous cardiac monitor
- Assess risk of future adverse cardiovascular events and death using GRACE Score.
- Consider nitrate to relieve cardiac pain or to treat acute heart failure if necessary. Start with isosorbide mononitrate 20mg bd using asymmetric dose at 8am and 2pm, reserving Nitrocine IV 1-10mg/hr for ongoing ischaemia/pulmonary oedema.
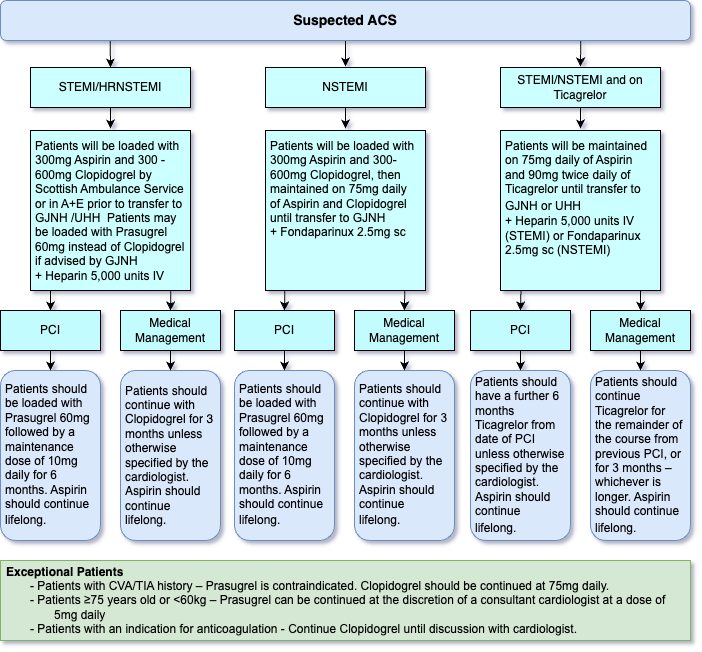
- Flowchart for suspected ACS is as follows:
Initial Management – If Taking DOAC or Warfarin
- Suspend DOAC/warfarin at front door and treat with aspirin 300mg then 75mg daily, clopidogrel 300mg then 75mg daily and fondaparinux.
- Start fondaparinux 2.5mg daily 24 hrs after last DOAC dose (or when INR drops <2 if on warfarin). If CrCl <20ml/min switch to enoxaparin 1mg/kg SC od.
- If clinically stable GJNH may defer taking patient for 48 hours if they have been taking a DOAC.
- If clinically unstable GJNH will take patient immediately even if they have been taking a DOAC.
- Patient can restart DOAC post angio with DAPT regimen decided by operator.
- If not for angio, then restart DOAC/warfarin with single antiplatelet agent (usually clopidogrel) for 6 months before going back to DOAC alone.
- Otherwise management is the same as for patients who are not taking an anticoagulant – see above
Management if Already on Ticagrelor
- Load with aspirin 300mg, Fondaparinux 2.5mg & Heparin 5000 units
- Maintain on aspirin 75mg once daily and Ticagrelor 90mg twice daily until transfer to Golden Jubilee National Hospital.
- If has PCI, patient should have further 6 months Ticagrelor from date of PCI unless otherwise specified by Cardiologist. Aspirin should continue lifelong.
- If medical management only, patient should continue Ticagrelor for the remainder of the course from previous PCI or for 3 months, whichever is longer. Aspirin should continue lifelong.
Further Management
- Refer to cardiologist/transfer to cardiology ward (D8)
- Refer Cardiac rehabilitation – phone 32130
- Cardiology will offer early coronary angiography and revascularisation to patients at medium or high risk of early recurrent cardiovascular events if no contraindication to angiography eg active bleeding or comorbidity
- Consider pre discharge stress testing in low-risk ACS patients who have been managed conservatively without inpatient coronary angiography.
- Provide information to patients and carers, listen to them and provide support at every stage of their journey
- Counsel patients regarding lifestyle changes including smoking cessation, exercise and diet
Aim to Discharge on
- Aspirin 75mg od
- Clopidogrel 75mg od for 3 months.
- Beta-blocker eg bisoprolol 2.5-10mg od
- Statin eg simvastatin 40mg at night but consider high dose atorvastatin 80mg in younger high risk patients
- ACE inhibitor eg Ramipril 2.5-10mg daily
-
Epleronone 25-50mg od if LVSD with EF <40% or diabetes
Flowchart for NSTEMI
Links
Content by Chris Isles and Alison Crooks