Home | Articles | Intravenous Fluids |
IV Fluid Prescription in Adults
Last updated 16th April 2024
Introduction
- Fluid prescriptions are very important. Prescribing the wrong type or amount of fluid can do serious harm
- Assessment of fluid requirements needs care and attention, with adjustment for the individual patient. This is as important as safe drug prescribing – fluids are drugs.
- Try to prescribe fluids during daytime ward rounds for patients you know rather than leaving it to the night teams. However, complex patients need review of fluid requirements more than once a day.
Exclusions
- Children under 16: Consult paediatrician.
Special Circumstances: Principles Remain the Same
- Burns: Use established protocols for burns.
- Diabetes: Use Diabetic Ketoacidosis (DKA) or hyperosmolar hyperglycaemic state protocols or use 0.18%NaCl/4%glucose/KCl with intravenous insulin.
- Obstetrics: Consult senior for complex patients.
- Head injury: Avoid fluids containing glucose.
- Renal/liver failure: Consult senior doctor.
Basic Physiology of Sick Patients
- It is easy to give an excess of salt and water but very difficult to remove them. Serum sodium may fall due to excess water load. Inadequate filling may lead to poor organ perfusion.
- In sick patients with leaky capillaries fluid retention contributes to organ dysfunction, resulting in complications such as ileus, poor mobility, peripheral oedema, pressure sores, pulmonary oedema, poor wound healing and anastomotic breakdown.
- Urine output naturally decreases during illness or after trauma (including surgery) due to increased sodium retention by the kidney. Too much intravenous fluid makes this worse. Cellular dysfunction and potassium loss result. Excess chloride leads to renal vasoconstriction and increased sodium and water retention. Urine output is a poor guide to fluid requirements in sick patients and oliguria does not always require fluid therapy (full assessment is required).
Questions to Ask Before Prescribing Fluid
- Is my patient euvolaemic, hypovolaemic or hypervolaemic?
- Does my patient need IV fluid and if so why?
- How much?
- What fluid does my patient need?
Is my Patient Euvolaemic, Hypovolaemic or Hypervolaemic?
- Euvolaemic: veins are well filled, extremities are warm, blood pressure and heart rate are normal.
- Hypovolaemic: often more difficult to determine than you might think. Easy if patient complains of thirst, has cool peripheries, respiratory rate >20, systolic BP<100mmHg, HR >90bpm, postural hypotension, oliguria and confusion. There may be history of fluid loss or low intake. Fall in heart rate with increase BP after 45˚ passive leg raise suggests hypovolaemia. Urea:creatinine ratio >100:1 suggests hypovolaemia. Weight and urine input/output charts are notoriously inaccurate. Signs of hypovolaemia may be unreliable in elderly patients. Consider urinary catheter in sick patients.
- Hypervolaemic: Patient is oedematous, may have inspiratory crackles, high JVP and history/charts showing fluid overload.
Does my Patient Need IV Fluid and if so Why?
- NO: Is patient drinking adequately, or receiving adequate fluid via NG feed or TPN? Is the patient receiving large volumes with drugs or drug infusions or a combination? Is the patient hypervolaemic: may need fluid restriction or gentle diuresis.
- YES: not drinking, has lost, or is losing fluid.
- Maintenance fluid only – patient does not have excess losses above insensible loss/urine. If no other intake he needs approximately 30ml/kg/24hrs. Patient may only need part of this if receiving other fluid. Patients having to fast for over 8 hours should be started on IV maintenance fluid.
- Replacement of losses, either previous or current. If losses are predicted it is best to replace these later rather than give extra fluid in anticipation of losses which may not occur. This fluid is in addition to maintenance fluid. Check blood gases.
- Resuscitation: The patient is shocked as a result of dehydration, blood loss or sepsis and requires urgent correction of intravascular depletion to correct the deficit.
How Much Fluid?
- Think Maintenance +/- Replacement +/- Resuscitation
- Maintenance fluid requirement approximately 30ml/kg/24hours.
- Replacement fluid requirement is often an intelligent guess
- Resuscitation fluid requirement is approximately 30ml/kg asap starting with a 500ml bolus
- Note urine does not need to be replaced unless excessive (diabetes insipidus, recovering renal failure).
- Post-op: high urine output may be due to excess fluid; low urine output is common and may be normal due to anti-diuretic hormone release.
Maintenance Fluid
- If no other intake a patient needs approximately 30ml/kg/24hrs. They may only need part of this if receiving other fluid. Patients having to fast for over 8 hours should be started on IV maintenance fluid.
- IV fluid should be given via volumetric pump if a patient is on fluids for over 6 hours or if the fluid contains potassium.
- Always prescribe as ml/hr not ‘x hourly’ bags.
- Never give maintenance fluids at more than 100ml/hour.
- Do not ‘speed up’ bags; rather give replacement for losses.
Weight (kg) Fluid Requirement mL/24hrs Rate mL/hr 35-44 1200 50 45-54 1500 65 55-64 1800 75 65-74 2100 85 ≥75 2400 100 (max) - Preferred maintenance fluids: 0.18%NaCl/4%glucose with or without added potassium (40mmol) in 1000ml .
- This fluid if given at the correct rate (Table) provides all water and Na+/K+ requirements until the patient can eat and drink or be fed. Excess volumes of this fluid (or any fluid) may cause hyponatraemia.
- Alternative maintenance fluid prescription could be dextrose 5% 500ml x3 with saline 0.9% 500ml plus added potassium (this is what we used to give)
- If serum sodium ≤132mmol/l use Hartmanns for maintenance.
- For the frail elderly, patients with renal impairment or cardiac failure and patients who are malnourished or at risk of refeeding syndrome consider giving less fluid: 20-25ml/kg/ day (NICE guidelines).
- If the serum potassium is above 5mmol/l or rising quickly do not give extra potassium.
- Give Pabrinex IV if refeeding risk.
- Diabetes: use 0.18%NaCl/4%glucose/KCl with intravenous insulin at maintenance rates.
- Electrolyte Requirements Sodium 1 mmol/kg/24hrs (approx. 1x500ml 0.9%NaCl), Potassium 1 mmol/kg/24hrs (give 20mmol/500ml bag)
- Calories: 50-100g glucose in 24 hours to prevent starvation ketosis. Consult dietician if patient is malnourished.
- Magnesium, calcium and phosphate may fall in sick patients – monitor and replace as required.
Replacement Fluid
- Required for fluid deficits, ongoing losses and redistribution (short of shock). These are often difficult to quantify so the amount of replacement fluid prescribed often has to be an intelligent guess
- Fluid deficits and ongoing losses may be due to diarrhoea, vomiting, fistulae, drain output, bile leaks, high stoma output, ileus, blood loss, excess sweating or excess urine.
- Redistribution of fluid into the tissues due to leaky capillaries common in pancreatitis, sepsis, burns and abdominal emergencies.
- It is vital to replace high GI losses as these patients may develop severe metabolic derangement with acidosis or alkalosis. Hypochloraemia may occur with upper GI losses. Check blood gases in these patients.
- Hyponatraemia is common in the absence of large GI losses. Causes are too much fluid, SIADH or chronic diuretic use. Treatment of hyponatraemia is complex and requires senior input. A sodium of < 125mmol/l is dangerous. 0.9%NaCl or fluid restriction are first line treatments and frequent U&Es are required. Link to page on Hyponatraemia.
- A normal potassium level does not mean that there is no total body potassium deficit. Give potassium in maintenance fluid. 10mmol/hour is safe to give through peripheral vein. 20mmol/hour can be given through large peripheral vein with ECG monitoring. Only in critical care areas give up to 40mmol in 100ml bags via a central line at 25-50ml/hr. Potassium-containing fluids must be given via a pump. Give Sando-K orally if possible. Link to page on Hypokalaemia.
- Estimate replacement fluid/electrolyte requirements by adding up all the losses over the previous 24 hours and give this volume as Hartmanns. Use 0.9% NaCl with KCl for upper GI or bile loss (high NaCl content). Otherwise avoid 0.9% NaCl as it causes fluid retention. Diarrhoea may lead to potassium loss.
Fluid Content/L Na K Cl Mg Ca Other Osm. 0.9%NaCl 154 0 154 0 0 0 308 0.18%NaCl 4% Glucose ± K 30 0 30 0 0 Gluc 40g/L 284 0.45NaCl 5% Glucose 77 0 77 0 0 Gluc 50g/L 406 Gelaspan 151 4 103 1 1 Acetate 24 284 Hartmann's 131 5 111 0 2 Lactate 29 274 PlasmaLyte 148 (PL148) 140 5 98 1.5 0 Acetate 27 297 5% Glucose 0 0 0 0 0 Gluc 50g/L 278
Resuscitation Fluid
- Resuscitation fluid requirement is approximately 30ml/kg asap starting with a 500ml bolus
- Resuscitation fluid is required for shock as a result of dehydration, blood loss, sepsis or anaphylaxis.
- Patients with significant co-morbidities and those taking cardiovascular drugs may decompensate with little fluid loss, while young, fit patients will compensate for much greater loss of intravascular volume
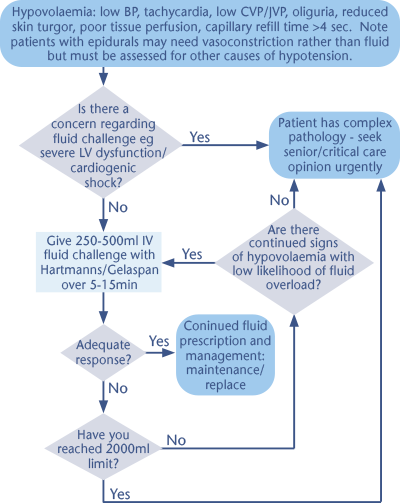
- For urgent resuscitation use Hartmann’s or colloid (Gelaspan/Albumin). Hartmann’s is a balanced electrolyte solution and is better handled by the body than 0.9%NaCl. Avoid Gelaspan in sepsis and consider Albumin only in patients with severe sepsis – See Fluid Challenge Algorithm
- Priorities: Stop the bleeding: consider surgery/endoscopy. Use Major Haemorrhage Protocol. Treat sepsis. CALL FOR HELP!
- For severe blood loss initially use Hartmann’s (or colloid) until blood/ clotting factors arrive. Use O Negative blood for torrential bleeding. Severely septic patients with circulatory collapse may need inotropic/vasopressor support. Their blood pressure may not respond to large volumes of fluid; excessive volumes may be detrimental.
Consider Critical Care Referral if:
- GCS ≤8 or falling from higher levels
- SpO2 <90% on 40% oxygen
- PaCO2 >7kPa unresponsive to NIV
- Persistent hypotension and/or oliguria unresponsive to 2000ml fluid/or concern over cardiac function
- Metabolic acidosis: base deficit -8 or worse, bicarbonate <18mmol/l, lactate >3mmol/l and not improving in 2 hours
- Aggressive/agitated patients whose treatment (e.g. oxygen/IV therapy) is compromised due to agitation.
- NB Referral is not always appropriate –consult senior doctor.
Links
- Guidance on IV Fluid and Electrolyte Prescription in Adults[pdf]
- A Brief Guide to Intravenous Fluid in Adults[pdf]
Content updated by Chris Isles.
