In this section : Renal
Kidney Biopsy Complications
Parenteral Iron for Non-HD CKD Patients
Management of uncomplicated Henoch-Schonlein Purpura (HSP) in under 16s
Prescribing Advice on Admission – Insulin
Sodium Glucose Transporter 2 Inhibitors (SGLT2i)
Gentamicin in Renal Replacement Therapy
Vancomycin in Renal Replacement Therapy
Haemodialysis Medication Prescribing
Contrast Associated AKI
Acute Kidney Injury – Introduction
Low Molecular Weight Heparin
Fluid Replacement in AKI
Management of Urinary Symptoms
Management of Acute Kidney Injury
Urinary Tract Infection
Urethral Catheterisation
Renal Transplants
Ureteric Colic & Renal Stones
Intravascular Catheter Related Blood Stream Infection
Care of Vascular Access
Urinary Incontinence
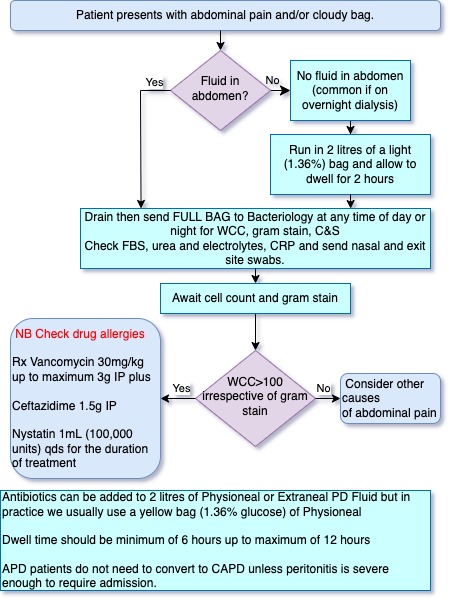
Peritoneal Dialysis Related Peritonitis
Peritoneal Dialysis Related Peritonitis
Last updated 22nd March 2024
Definitions
- Peritoneal dialysis associated peritonitis is diagnosed when at least 2 of the following are present:
- Clinical features consistent with peritonitis, i.e. abdominal pain and/or cloudy dialysis effluent
- Dialysis effluent white cell count > 100/microlitres or > 0.1 x 109/L (after a dwell time of at least 2 hours), with more than 50% polymorphonuclear leucocytes
- Positive dialysis effluent culture
- ***We recommend that PD patients presenting with cloudy effluent be presumed to have peritonitis and treated as such until the diagnosis can be confirmed or excluded***
- Relapsing peritonitis is defined as further episode of peritonitis caused by the same organism (or sterile culture), occurring within 4 weeks of completing antibiotic therapy for peritonitis.
- Repeat peritonitis is a further episode of peritonitis more than 4 weeks after completing antibiotics, with the same organism.
- Recurrent peritonitis is a further episode of peritonitis caused by a different organism, occurring within 4 weeks of completing antibiotics for peritonitis.
- Outcome following an episode of peritoneal dialysis related peritonitis an outcome must be documented on SERPR. Outcomes are classified as:
- Cure defined as resolution of evidence of peritonitis following antimicrobial therapy and without the need for catheter removal.
- Peritoneal dialysis catheter removal.
- Patient death This includes patients who die within 28 days of presentation of peritonitis even if the effluent WCC had cleared.
Diagnosis (Day 0)
The following should be performed:
- Initial Assessment:
- Routine observations (temperature, BP, pulse rate)
- PD effluent to bacteriology for URGENT white cell count, Gram stain and culture and sensitivity
- Check CRP and consider blood cultures if febrile
- Record details of the initial assessment, including urgent white cell count result, in the case notes (or clinical portal) and clinical history on SERPR.
- Consider predisposing factors:
- Exit site or tunnel infection
- Break in sterile dialysis procedure or equipment (without subsequent administration of prophylactic antibiotics)
- Diverticulosis or other bowel disease
Initial Antimicrobial Therapy (Day 0)
- The aim of initial therapy is to provide cover against both gram positive and negative organisms. Vancomycin provides gram positive cover. Ceftazidime provides gram negative cover. Antibiotics should be given via an intraperitoneal route. Details of alternative antibiotics for patients with confirmed allergies to these antibiotics are provided below.
- All intermittent (bolus) intraperitoneal (IP) dosages of antibiotics should be administered via peritoneal dialysis exchanges with a minimum dwell time of 6 hours. IP antibiotics are compatible with Icodextrin (Extraneal) dialysis fluid.
- The loading dosages of intraperitoneal vancomycin and ceftazidime are as follows:
- Vancomycin – 30mg/Kg body weight to a maximum of 3g intraperitoneally in a minimum 6hr dwell.
- Use a vancomycin prescription chart to record doses administered and subsequent vancomycin levels. Doses given should also be documented in HEPMA. If a patient has a confirmed allergy to vancomycin then daily IP teicoplanin should be used instead. See page 7.
- Ceftazidime – 1.5 g intraperitoneally in a minimum 6 hr dwell. Administer daily
- If the patient has an allergy to ceftazidime or has had a previous known Clostridium difficile infection then aztreonam should be used instead. See page 7.
- Treatment should start immediately after the effluent white cell count is found to be greater than 100/μl. Automated Peritoneal Dialysis (APD) patients require a continuous ambulatory peritoneal dialysis (CAPD) exchange, with antibiotics added.
- Note: APD patients do not need to convert to CAPD but, if peritonitis is severe enough to require inpatient stay APD patients should be converted to CAPD.
Management on Day 1
- The following should be done:
- Routine observations (temperature, BP, pulse rate)
- Record white cell count on overnight or long day dwell dialysate effluent in the case notes (or clinical portal) and on SERPR.
- Administer 1.5g ceftazidime intraperitoneally in a long dwell (use aztreonam intraperitoneally if previous c.difficle infection or ceftazidime allergy – see below
- See below if teicoplanin is being used instead of vancomycin.
- Prescribe Nystatin 1 mL (100,000 Units) QDS for the duration of treatment to prevent fungal peritonitis.
Management on Day 2
- Routine observations (temperature, BP, pulse rate)
- Record white cell count on overnight or long day dwell dialysate effluent in the case notes (or clinical portal) and on SERPR.
- Check serum CRP and white cell count.
- Administer 1.5 g ceftazidime IP in a long dwell. (use aztreonam intraperitoneally if previous C.difficle infection or ceftazidime allergy – see below)
- If residual renal function >5ml/min, check vancomycin level after 48hrs. Vancomycin and aminoglycoside levels fall more quickly in patients with residual urinary output. Patients with significant residual renal function will require more frequent monitoring of serum vancomycin levels.
- Give vancomycin 15 mg/kg IP into long dwell when level <20mg/l (note different level to that used in haemodialysis). If level <10mg/l discuss with pharmacist/doctor as dose may require to be altered.
- See below if teicoplanin is being used instead of vancomycin.
Management on Day 3
- The following should be done:
- Routine observations (temperature, BP, pulse rate)
- Record white cell count on overnight dialysate effluent in the case notes (or clinical portal) and on SERPR.
- Check serum CRP and white cell count.
- Check vancomycin levels if residual renal function less than 5ml/min. Give vancomycin 15mg/kg IP into long dwell when level less than 20mg/l.
- Review bacteriology and clinical response (serial results of effluent WCC, CRP and serum vancomycin level)
- Review antibiotic regimen with microbiology results and in consultation with microbiology team
- If gram positive organism:
- Continue vancomycin 15mg/kg intraperitoneally (minimum 6 hour dwell) when vancomycin level falls below 20mg/l (See below) if teicoplanin is being used instead of vancomycin)
- If gram negative organism:
- Continue ceftazidime daily dosing, 1.5g intraperitoneally (minimum 6 hour dwell). Use aztreonam if ceftazidime allergy or previous c.difficle infection (see below)
- If multiple gram negative organisms and/or anaerobes:
- Consider surgery (likely intra-abdominal pathology)
- Add metronidazole
- If culture negative:
- Continue vancomycin (or teicoplanin) and ceftazidime (or aztreonam)
- If no clinical improvement:
- Most patients should be improving by 48 hours
- If not responding by 72 hours, consider:
- Check of antimicrobial sensitivities
- Tunnel infection or exit site infection (commonly Gram positive)
- Unusual organism – treat as per microbiology advice
- Catheter removal if dialysate WCC not decreasing
- Fungal infection – arrange catheter removal
- Recurrent Staphylococcus Aureus or persistent coagulase negative staphylococcus (from PD fluid) – add rifampicin 600 mg/day. NB rifampicin has many drug interactions see British National Formulary (BNF).
Management from Day 4 Onwards
- Continue vancomycin (or teicoplanin) and ceftazidime (or aztreonam) or change antibiotic therapy depending on bacteriology results.
- Review interval at the PD unit will depend on progress and the need to monitor WCC of effluent and serum levels of antibiotics
Management to minimise complications
- Treatment Duration
- Duration of treatment depends on clinical response and is usually at least 14 days. Longer duration of treatment (21 days) is required for more severe infections caused by Staphylococcus Aureus and Gram negative organisms.
- Ultrafiltration
- Ultrafiltration may be affected by peritonitis. PD regimens may need altered to maintain adequate fluid removal. Icodextrin (Extraneal) is useful in maintaining net ultrafiltration volumes. Occasionally heparin (500 units/litre) may need to be added to the PD fluid, if there is fibrin in the effluent.
- Catheter Removal
- Consider catheter removal after a first episode of recurrent peritonitis .
- If catheter removal is required, appropriate IV or oral antibiotics and/or antifungal drugs should continue to be prescribed.
Alternative Antibiotics
- Treatment should be standardised and in line with these guidelines wherever possible. A comprehensive list of alternative antibiotics is available via ISPD. The use of non-standard anti-microbial therapy is best discussed with senior medical and microbiology staff.
- Use of Intra-Peritoneal Teicoplanin
- Teicoplanin has gram positive organism cover and should be used in place of vancomycin where there is a documented vancomycin allergy.
- Teicoplanin Dosing Regimen:
- Day 0 400mg IP once only
- Day 1-7 20mg/litre into each exchange
- Day 8-14 20mg/litre into alternate exchanges
- Day 15-21 20mg/litre into overnight exchanges
- It is recommended to use 200mg vials and reconstitute with 3ml water provided then further dilute with 2ml sodium chloride injection. This gives 200mg in 5ml which is 40mg/ml. Then inject 1ml in each 2 litre exchange.
- Once reconstituted – vial stable for 24hr. In the event that only 400mg vials of teicoplanin are available: reconstitute as above but only inject 0.5ml into each 2 litre exchange.
- Use of Intra-Peritoneal Aztreonam
- Aztreonam has gram negative organism cover and should be used in place of ceftazidime where there is a documented ceftazidime allergy or when the patient has a history of a previous c.difficle infection.
- Aztreonam Dosing Regimen:
- Day 0- 21 Administer 3g daily intraperitoneally in a minimum 6 hour dwell
- Use of Intra-Peritoneal Gentamicin
- Gentamicin should only be used in conjunction with advice from senior medical and microbiology staff.
- Gentamicin Dosing Regimen:
- Intermittent – (in 2 litre exchange with a dwell time of at least 6 hours) Dosage – One exchange a day – 0.6 mg/kg body weight for 14 days Dosage monitoring – to avoid toxicity serum gentamicin levels should be monitored at 24 hours and 48 hours along with effluent WCC and culture. Further dose may be required if level is < 2, the result should be interpreted in the light of the time period between dose and blood level.
(Contamination of PD system – prophylactic antibiotics (Vancomycin 1g + Ceftazidime 1.5g IP or Teicoplanin if allergic to vancomycin or Aztreonam if allergic to penicillin) should be administered after wet contamination of the PD system to prevent peritonitis.)
 Links
Links
Content Updated by Dr Elaine Rutherford & Dr Thalakunte Muniraju. Adapted with permission from NHS GGC Guidelines 2018.
