In this section : Alcohol Withdrawal
Alcohol Withdrawal
Home | Articles | Alcohol Withdrawal |
Alcohol Withdrawal
Last updated 3rd December 2020
Updated on 6th August 2020.
THESE GUIDELINES ARE FOR ALCOHOL WITHDRAWAL ONLY AND SHOULD NOT BE USED FOR BENZODIAZEPINE WITHDRAWAL. THE ADDICTION TEAM ARE WORKING ON A BENZO WITHDRAWAL PROTOCOL BUT IN THE MEANTIME WE ARE ADVISED TO FOLLOW THE SLOW WITHDRAWAL PROTOCOLS THAT CAN BE FOUND AT BENZO.ORG.UK
Inpatient referrals
- Refer to Addiction Liaison Service via Cortix or by phoning 33090
- Patients should be aged 18 or over and medically fit to be seen and engage with service
- Patients with alcohol withdrawal and suicidal ideation or significant mental health issues should be referred to Acute Liaison Psychiatry as well as Addiction Liaison Service
- Patients discharged before they can be seen by Addicton Liaison eg at weekends should be given number for NHS Drug and Alcohol Service – 01387 244555
- Patients presenting with cannabis/cocaine/other recreational drug use rather than alcohol withdrawal should be referred to Addaction for follow up following discharge – 01387 263208 (Dumfries) or 01776 705907 (Stranraer).
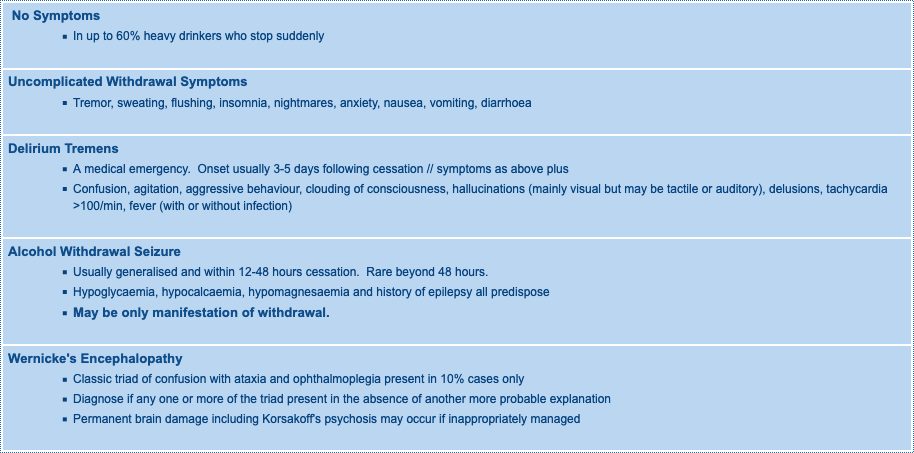
Alcohol Withdrawal Syndromes
- Alcohol withdrawal usually begins within 6-8 hours after an abrupt reduction in heavy drinking
- Can be earlier in severe dependence or may not manifest for up to 72 hours
- Can develop before the blood alcohol level has fallen to zero.
- Generally peaks within 10-30 hours and lasts for 3-7 days
Alcohol Withdrawal Syndromes
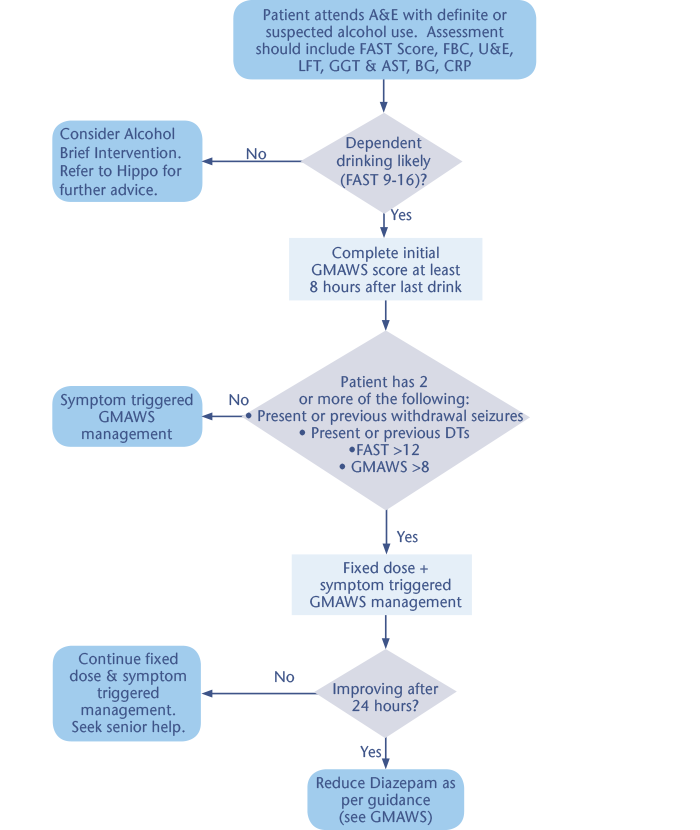
Assessment and General Management
- Calculate alcohol intake- see below
- Screen for dependence – FAST score – see below
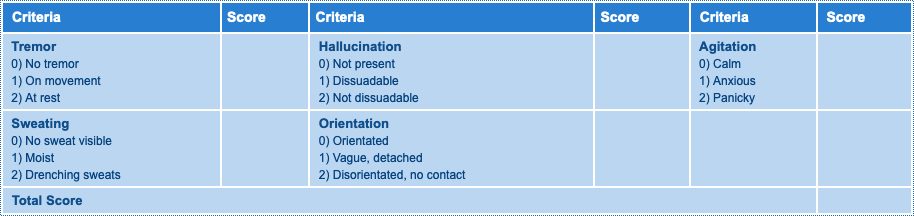
- Assess severity of withdrawal using Glasgow Modified Alcohol Warning Score (GMAWS) – see below
- Look for stigmata of chronic liver disease
- Consider other possible causes of confusion in an alcohol dependent patient – see below
- Check FBC, U&E, LFTs including GGT & AST, BG, CaPO4, Mg and coag screen, blood alcohol level may also be useful.
- Maintain 2-2.5litres intake per day using IV if necessary
- Ensure good lighting and cool ambient temperature, good ventilation, supportive nursing, reassurance, single room if confused
- Consider ear plugs if difficulty sleeping (can be sourced from H@N Nurses)
- Prescribe Pabrinex and Benzodiazepines as per protocol
Possible Causes of Confusion in an Alcohol Dependent Patient
- Acute alcohol intoxication
- Alcohol withdrawal including Delirium tremens
- Hypoglycaemia
- Head injury
- Subdural haematoma
- Wernicke’s encephalopathy
- Hepatic encephalopathy
- Septicaemia
- Meningitis including TB meningitis
- Concurrent illicit substance abuse.
Calculating Alcohol Intake
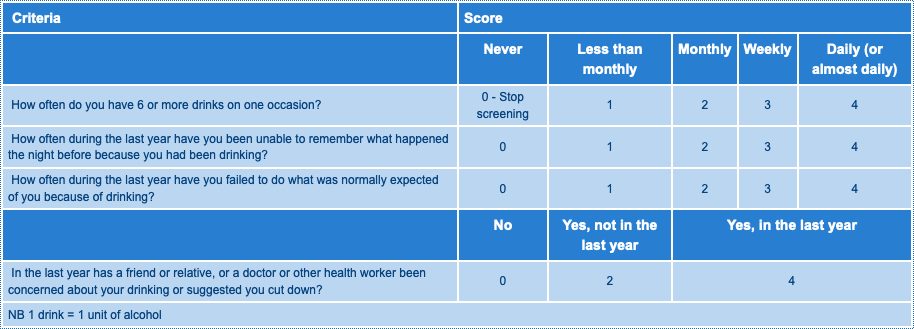
Fast Alcohol Screening Tool – FAST
What to do about the FAST Score
- FAST score 0-2: No action required
- FAST score 3-8: Advise regarding safe drinking levels and offer information leaflet/advice.
- FAST score 9-16: Probable dependent drinking. Advice as above and consider referral to Alcohol Liaison Nurse.
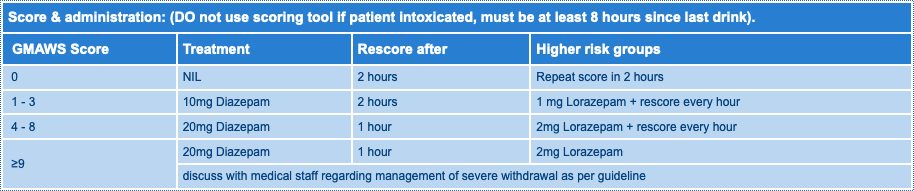
Glasgow Modified Alcohol Warning Score (GMAWS) Screening Tool
Symptom Triggered GMAWS Management
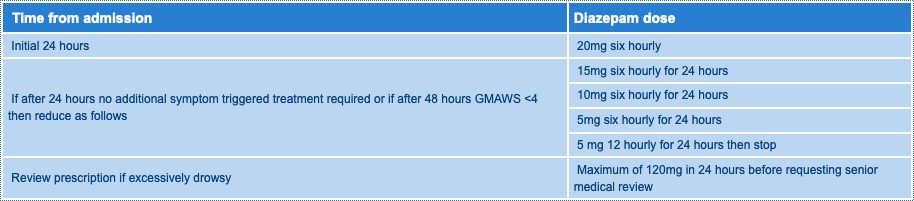
Fixed Dose Diazepam Regimen
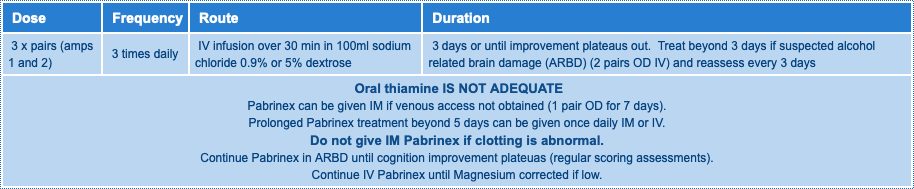
Pabrinex Protocol for Alcohol Withdrawal
- The guidance applies to all patients with signs of alcohol withdrawal
- It includes chronic alcohol users who are dependent on alcohol but also those who have a hazardous/harmful alcohol intake.
- Patients MUST be given Pabrinex® BEFORE the administration of glucose or nutritional support
- Intravenous Pabrinex® should be administered over 30 minutes
- Anaphylaxis is a rare complication of IV Pabrinex® administration and even less common with IM administration. Monitor the patient for wheeze, tachycardia, breathlessness and skin rash. Facilties for the administration of adrenaline and other resuscitation should be available.
- Further vitamin supplementation as clinically indicated by responsible medical team in the context of a general nutritional assessment.
Use Lorazepam for Higher Risk Groups
- Patients with evidence of liver disease, especially jaundice, ascites, encephalopathy
- Patients with other co-morbidities eg COPD, pneumonia, cerebrovascular disease, head injury, reduced GCS, elderly over 70 years, head injury.
- Patients with co-prescribed CNS sedative drugs eg opiates
- Use oral lorazepam in these groups in a symptom-triggered fashion: 1-2mg to a maximum of 12mg in 24 hours before requesting senior medical review. Give IM or SC if unable to swallow.
- Patients on lorazepam may require more frequent monitoring and PRN doses due to shorter half life
Aggressive/uncontrollable/dangerous behaviour
-
- Move patient to Critical Care
- Follow dosing schedule for IV diazepam or IV lorazepam in table below
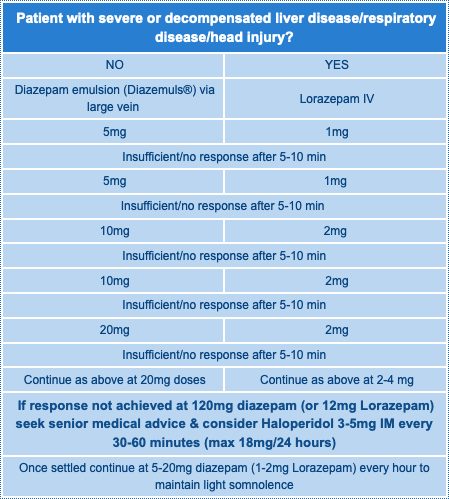
- Have flumazenil available
- Diazepam 120mg or lorazepam 12mg over 24 hours is unlikely to cause problems in an uncomplicated patient
- Consider adjunctive therapy with haloperidol 3-5mg IV or IM (smaller doses unlikely to be effective) if still not settling (minimum 4 hourly, max 12-18mg/24 hours)
- Once settled continue 5-20mg diazepam (1-2mg lorazepam) per hour to maintain light sedation
- Give Pabrinex 3 pairs ampoules IV
- Consider need for glucose and magnesium, but do not give glucose until after Pabrinex.
- In extreme cases where very high dose parenteral diazepam >200mg is ineffective it may be necessary to incubate.
Patients Unable to Tolerate Oral Medication
- Patients unable to tolerate oral medication may receive IV therapy (Diazemuls or lorazepam) as an alternative at 50% of the oral dose in the first instance and response assessed.
- It is recommended that IV benzodiazepines are administered by an experienced member of staff (FY2 or above).
Monitoring
- All patients should be closely observed for signs of oversedation
- Higher risk groups (see above), patients with severe withdrawal and patients requiring intravenous or intramuscular sedation require close monitoring (pulse, blood pressure, respiratory rate, GCS, oxygen saturation), ideally with one-to-one nursing care.
- Consultation regarding intensive care support may be necessary in extreme situations.
- If patient is only on symptom triggered GMAWS and is scoring 3 or less after 72 hours then symptom triggered treatment can be stopped
Approximate Oral Benzodiazepine Equivalence
- 10mg diazepam = 1mg lorazepam = 30mg chlordiazepoxide.
Medication on Discharge
- Do not discharge on regular benzodiazepine unless arrangement confirmed with community addiction services or Alcohol Liaison Nurse. See Hippo (link below) for advice on discharging detox patients.
- Chlordiazepoxide is the recommended benzodiazepine for community use.
- All patients should go home on Thiamine 50mg qds.
Summary Management of Alcohol Withdrawal