In this section : Respiratory
Croup
Bronchiolitis
Acute Wheeze or Asthma in Paediatrics
Inhalers for Adults with Asthma
Greener Inhaler Prescribing
Bi-Level NIV S/T Guidelines for CCU Phase
Bi-Level NIV S/T Guidelines for ED Phase
Chronic Cough Pathway
Paediatric Bronchiolitis
Exacerbation of COPD
Chronic Obstructive Pulmonary Disease
Legionnaires Disease
Interstitial Lung Disease
Oxygen Therapy
Acute Asthma
Pleural Effusion
Spontaneous Pneumothorax
Community Acquired Pneumonia (CAP)
Breathlessness with Abnormal CXR
Home | Articles | Respiratory |
Community Acquired Pneumonia (CAP)
Last updated 3rd March 2022
Causes
- Strep pneumoniae 40%, Influenza A and B 10%, H influenzae 5-10%. All other causes uncommon eg legionella, staph, gram neg and atypicals.
- Mycoplasma peaks in 4 year cycles, otherwise uncommon.
- H influenzae and M catarrhalis may be more common in COPD patients
- Bacterial causes only found in 25% cases admitted to hospital, so treatment usually empirical
- Aspiration is an important risk factor for CAP in elderly patients esp nursing home residents
Clinical Features
- Cough, spit, fever, pleuritic pain, dyspnoea, haemoptysis
- Extra pulmonary – confusion, diarrhoea, vomiting, abdo pain, paralytic ileus, myalgia, cerebellar & headache.
- Crackles commonest physical sign with bronchial breathing <33% cases
- Atypical presentations frequently occur in elderly in whom fever, cough and spit less common while confusion more common
Investigations
- SpO2 in all
- ABG as indicated
- CXR
- Routine bloods – FBC, U&E, LFTs, CRP
- Microbiology – see below
Severity Assessment of CAP in Hospital
- There is more to this than the CURB65 score! We currently recommend 3Cs – CURB65, Comorbidities and Clinical concerns – which allows us to classify pneumonia as mild, moderate or severe.
- Stratification allows a decision on microbiological testing and antibiotic therapy as shown below.
- If CURB65 is: 0 if under 65 years, or ≤1 if over 65 with no comorbidity or clinical concern, consider ambulatory care. Click here to see the Ambulatory Care Pathway for CAP.
| CURB65 Adverse Prognostic Features (Score 1 for each) | Confusion, new (MSQ ≤8/10) |
| Urea >7mmol/L (if available) | |
| Respiratory rate ≥30/min | |
| BP <90mmHg (systolic) or ≤60mmHg (diastolic) | |
| 65 Age ≥65 yrs | |
| Co-morbidities | Co-existing chronic illness |
| Clinical concerns | Pulse oximetry <92% or PaO2 <8 kPa on any FiO2 (if available) |
| Bilateral or multi-lobar changes on CXR |
Microbiology
The extent to which we investigate pneumonia microbiologically will be determined by severity of pneumonia. The options and when to request them are as follows:
| No microbiological tests required | Mild |
| Consider sputum for mycoplasma PCR, viral throat swab for influenza PCR | During outbreaks |
| Sputum C&S, Blood culture, urine for pneumococcal & leghionella antigen | Mod/Severe |
| Pleural fluid for microscopy, culture and pneumococcal antigen | If present |
| Consider sputum/throat swab PCR for respiratory viruses and atypical pathogens - mycoplasma, chlamydia, Q fever, influenza | Severe |
| Tests for Legionella if Legionella suspected - urine for Legionella antigen and sputum for Legionella culture/direct IF | Severe if risk factors |
| Consider bronchial washings | Severe if failing to improve |
| Blood for HIV | All bacterial pneumonia |
Management
- Assess severity by CURB65, Comorbidities and Clinical Concerns
- Oxygen – see below
- Antibiotic within 4 hours of admission, see flow chart
- IV Fluid if volume deplete, aiming for SBP >90mmHg and UV >30ml/hr
- Physiotherapy if copious secretions
- Low molecular weight heparin if not fully mobile
- Analgesia for pleuritic pain – NSAIDs unless contraindicated
- Repeat CXR and CRP if not improving within 3 days.
- Treat complications eg chest drain if pleural fluid turbid/low pH
- Refer Respiratory team/move to HDU/consider ITU if severe/not improving
Oxygen
- Aim for SpO2 94-98% and PaO2 >8kPa in patients who are not at risk of hypercapnic respiratory failure. High flow oxygen safe in this group
- In COPD patient give 2l/min initially, aim for SpO2 88-92% then take ABGs to ensure not hypercapnic.
Antibiotics
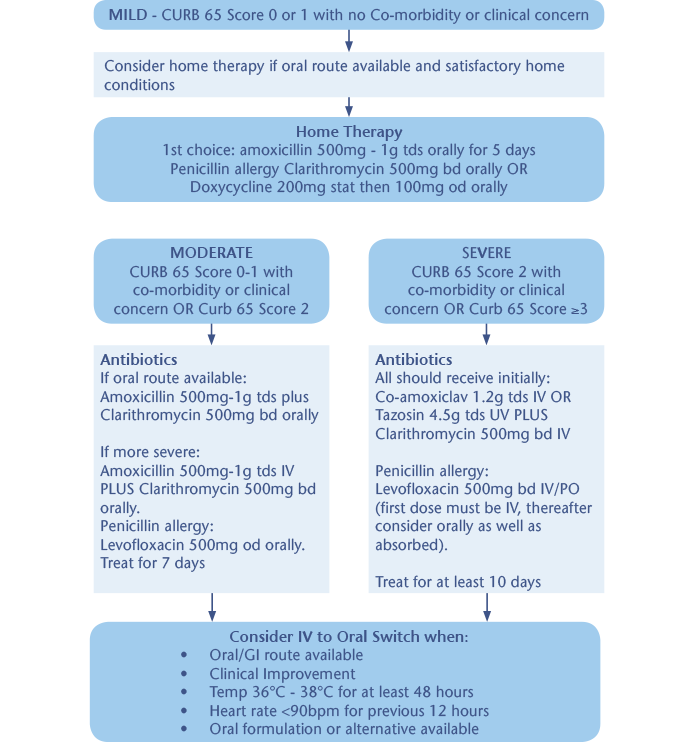
- Antibiotic therapy is the cornerstone of management but over use may be harmful eg C. diff diarrhoea and antibiotic resistance.
- Target should be to offer antibiotics as soon as possible after diagnosis and certainly within 4 hours to all patients with CAP who are admitted to hospital.
- If diagnosis is uncertain then it is acceptable to withhold antibiotic if CRP <20 pending senior review (but don’t withhold antibiotic if diagnosis certain just because CRP is low initially).
Reasons for Failure to Improve
- Wrong diagnosis – commonly one of:
- PE
- Pulmonary oedema
- Bronchial carcinoma
- Bronchiectasis
- Wrong antibiotic – atypical pathogen/resistant organism
- Wrong dose of correct antibiotic/poor absorption orally
- Impaired host defences – local eg aspiration or systemic eg myeloma
- Complications of CAP – esp effusion, empyema, abscess
- Overwhelming infection
- Improvement expected too soon esp in elderly
Refer to ITU If
- PaO2<8.0kPa despite high FiO2.
- Progressive hypercapnia,
- H+ >50
- Shock or depressed GCS <8
What to Tell Patients
- Most patients will be unaware of the timeline for recovery following CAP
- 1 week – fever should have resolved
- 4 weeks – chest pain and sputum production should have reduced substantially
- 6 weeks – cough and breathlessness should have improved significantly
- 3 months – most symptoms should have resolved but fatigue may still be present
- 6 months – most people will feel back to normal
- They should know to contact their GP if their condition deteriorates following discharge from hospital or if their recovery is slower than indicated above.
When is it Safe to Discharge?
- Safe to go home when: –
- Temp <37.5
- Respiratory rate <24/min
- Heart rate <100/min
- SBP >90mmHg
- SpO2 >90% on room air
- Normal mental status
- Able to eat without assistance
- Should delay discharge if 2 or more of the above cannot be satisfied.
Follow Up
- CXR need not be repeated before discharge if making good clinical recovery
- The hospital doctor should arrange repeat CXR as outpatient at about 3-4 weeks following discharge to ensure resolution
- Consider further tests including bronchoscopy in patients with persisting clinical or radiological signs at this time
- Offer influenza and pneumococcal vaccination to at risk individuals as per Dept of Health guidelines
- Offer smoking cessation advice to all smokers with CAP
