In this section : Haematology and Thrombosis
Myeloma
Warfarin
Anticoagulation for AF, DVT and PE
Orthopaedic VTE Risk Assessment
Haemolytic Anaemia
Platelet Transfusion
Parenteral Iron in Adults >18 Years
Pulmonary Embolism
Deep Vein Thrombosis of Lower Extremities
Bleeding with Other Antithrombotics
Low Molecular Weight Heparin
Haematinic Testing
Thromboprophylaxis for Non-Covid Patients
Thrombophilia Screening
Antithrombotics in Hip Fracture
Reversal of Warfarin
Lumbar Puncture, Antiplatelet & Anticoagulant Drugs
Antithrombotics & Surgery
Iron Deficiency Anaemia
Unfractionated Heparin Infusion
Massive Pulmonary Embolism
Deep Vein Thrombosis of Lower Extremities
Last updated 30th June 2023
Diagnostic Algorithm for Suspected DVT
- Pre-test probability determines whether next test should be D-Dimer or Doppler scan – see flow chart
- The definitive test for DVT is full colour doppler US venogram including calf veins and tender areas and spectral doppler to check there is no iliac occlusion
- Note that the Wells’ Score for DVT is different for the Wells’ Score for PE.
Pre-Test Probability – Wells’ Clinical Score
| Risk Factor | Score |
| Active cancer (treatment ongoing or within the previous 6 months or palliative) | 1 |
| Paralysis, paresis or recent plaster immobilisation of the lower extremities | 1 |
| Recently bedridden for more than 3 days, or major surgery within 12 weeks | 1 |
| Localised tenderness along the distribution of the deep venous system | 1 |
| Entire leg swollen | 1 |
| Calf swelling by more than 3cm when compared to the asymptomatic leg (10cm below the tibial tuberosity) | 1 |
| Pitting oedema (greater in the symptomatic leg) | 1 |
| Collateral superficial veins (nonvaricose) | 1 |
| Previously documented DVT | 1 |
| Alternative diagnosis as likely or more likely than that of deep vein thrombosis | -2 |
| Clinical Probability | |
| DVT Likely | ≥2 |
| DVT Unlikely | <2 |
D-Dimer
- DGRI use a highly sensitive assay with a cut-off level of >500ng/ml indicating an abnormally raised level.
- In addition to VTE, D-dimers will be raised in any condition that leads to increased production of thrombins: surgery, trauma, infection, inflammation, DIC, pregnancy and delivery, cancer, thrombosis/bruising
- D-dimers have high sensitivity (high neg predictive value) & low specificity (low pos predictive value) for VTE
- This means that a negative result in the presence of a low pre-test probability, nearly always excludes, but that a positive result cannot confirm a diagnosis of VTE
- The use of D-dimer in the diagnosis of DVT & PE is shown in the flow charts.
Flow Chart Summary
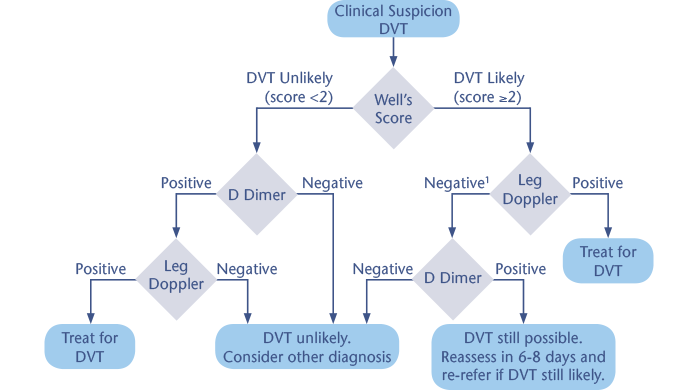
1Give a treatment dose of LMWH if leg doppler not available in 4 hours.
Initial Management of DVT
- Consider managing as outpatient if you can.
- Admission more likely to be required if:
- Chronic heart failure
- Suspected bilateral DVT
- Extremes of bodyweight
- Renal impairment with eGFR 30ml/min
- Severe pain
- Immobility
- Comorbidity
- If DVT likely AND admission not necessary then GP should give Apixaban 10mg bd and send to ED Consultant morning clinic between 1100-1130 next day.
- If scan positive, ED will start apixaban 10mg bd for one week, then 5mg bd for remainder of treatment. If a one-off dose of LMWH has been given then start treatment with apixaban when next treatment of LMWH would have been due – do not use LMWH and apixaban simultaneously – see Treatment of VTE for more information
- Patients who present directly to ED with swollen leg should go to medicine if they require admission
- Alternatively, Rx Fragmin and Warfarin remains acceptable if DOAC contraindicated or if preferred, though remember to continue Fragmin until INR therapeutic ie >2.0 for 48 hours.
- During initial ambulation and for at least 2 years the patient should be encouraged to wear TED stockings to reduce the instance of post phlebitic syndrome, unless contraindicated
DVT and Cancer
- Pease visit link to the Edinburgh Cancer Centre’s Antithrombotic Guidelines for guidance.
Wells’ Score ≥2, Positive D-Dimer and Negative Doppler
- GP should re-assess in one week and refer to ED Consultant morning clinic if signs persist or worsen.
Unprovoked DVT and Underlying Malignancy
- 10% patients with idiopathic DVT will have malignancy, often diagnosed in first 6 months after presentation
- Consider underlying maligancy if D-dimer >4000
- May be presenting sign of prostate or pancreatic cancer
- More frequently occurs late in the course of breast, lung, colon, uterine and brain cancer
- Recurrent thrombosis and abnormal clinical findings during an initial clinical evaluation are the most likely indicators of underlying malignancy
Assessment of Patients with Unprovoked DVT Should Include
- Offer all patients the following investigations for cancer
- Physical examination guided by the patients’ full history, and
- CXR, and
- FBC, U&E, LFTs & Calcium, and
- Urinalysis
- Consider further investigations for cancer with CT Abdo/Pelvis, and a mammogram in women, in all patients aged >40 with a first unprovoked DVT or PE who do not have signs or symptoms of cancer on initial investigation
DVT Mimics
- Baker’s cyst – Synovial cyst in popliteal fossa originating from knee, often associated with calf bruising. Confirm by ultrasound. Reduce knee effusion by analgesia, control arthritis if present, consider steroid injections & rest the knee. Interventions of no or little use include knee supports or aspiration/injection/excision of the cyst.
- Cellulitis – Leg often red with distinct margins & tender to touch. Please click here for the section on Cellulitis.
- Superficial Phlebitis – see below
- Haematoma – Suspect if bruising. Avoid anti-coagulants!
- Knee joint inflammation
- Oedema due to HF, nephrotic syndrome or immobilisation. Note nephrotic syndrome may also predispose to DVT. Worth checking urine for protein in all patients with DVT.
- Calf muscle tear or sprain – look for bruising.
- Chronic venous insufficiency – probably commonest cause of swollen leg. Clues include obesity and haemosiderin stain in gaiter area
Superficial Vein Thrombophlebitis
- Patients with lower limb SVT should have ultrasound assessment to exclude DVT, particularly if affecting the proximal long saphenous vein
- Patients with confirmed SVT within 3 cm of the saphenofemoral junction should be considered for therapeutic anticoagulation
- Patients with SVT and risk factors for extension, recurrence or progression should be offered treatment with prophylactic doses of LMWH for 30 days (currently an unlicensed indication) or fondaparinux for 30–45 days
- Other patients with SVT should be offered 8–12 days NSAIDs unless contraindicated
- Investigation of patients with SVT for underlying thrombophilia is not routinely indicated, and should follow existing guideline criteria.
